What is Glaucoma?
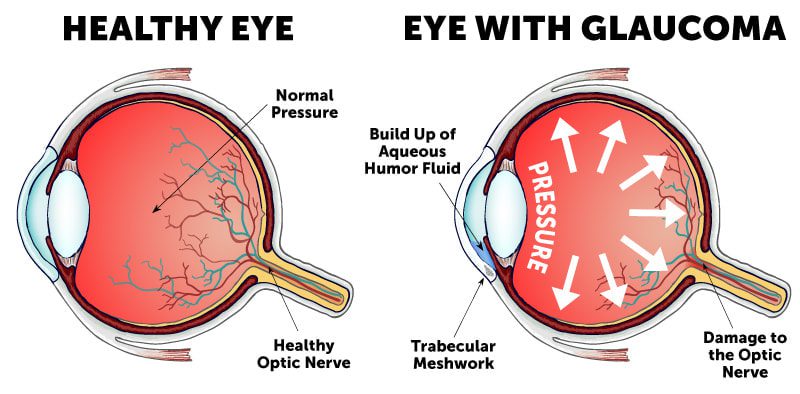
Glaucoma is a group of eye diseases that damage the optic nerve, typically caused by high intraocular pressure (IOP). It’s called the “silent thief of sight” because it often progresses without symptoms until significant vision loss occurs.
Key Facts (National Eye Institute [NEI]):
✔ Affects 3 million Americans (half unaware they have it)
✔ Second leading cause of permanent blindness worldwide
✔ Vision loss is irreversible but preventable with early detection
✔ Risk increases dramatically after age 60
Types of Glaucoma (American Academy of Ophthalmology [AAO])
- Primary Open-Angle Glaucoma (POAG) (Most Common – 90% of cases)
- Slow drainage of aqueous humor
- Develops gradually with no early warning signs
- Angle-Closure Glaucoma (Medical Emergency)
- Sudden blockage of drainage canals
- Causes rapid pressure buildup
- Normal-Tension Glaucoma
- Optic nerve damage despite normal IOP
- Linked to poor blood flow to optic nerve
- Secondary Glaucoma
- Caused by eye injury, inflammation, or medications
- Congenital Glaucoma (Rare)
- Present at birth due to abnormal eye development
Symptoms (Mayo Clinic)
Open-Angle Glaucoma:
- No early symptoms
- Gradual peripheral vision loss (tunnel vision in late stages)
Acute Angle-Closure Glaucoma (EMERGENCY):
- Severe eye pain
- Headache
- Nausea/vomiting
- Blurred vision
- Halos around lights
- Sudden vision loss
Diagnosis (AAO)
- Tonometry – Measures eye pressure (10-21 mmHg is normal)
- Ophthalmoscopy – Examines optic nerve damage
- Perimetry (Visual Field Test) – Maps peripheral vision loss
- Gonioscopy – Checks drainage angle
- Optical Coherence Tomography (OCT) – Detailed optic nerve imaging
Treatment (NEI)
1. Eye Drops (First Line Treatment):
- Prostaglandins (increase fluid outflow)
- Beta-blockers (reduce fluid production)
- Alpha-adrenergic agonists
- Carbonic anhydrase inhibitors
2. Oral Medications:
- Acetazolamide (for emergency pressure reduction)
3. Laser Treatments:
- Trabeculoplasty (for open-angle)
- Iridotomy (for angle-closure)
4. Surgical Options:
- Trabeculectomy (creates new drainage channel)
- Glaucoma drainage implants
- Minimally invasive glaucoma surgery (MIGS)
Prevention (CDC)
Regular comprehensive eye exams (every 2-4 years after 40, annually after 60)
Know family history (4-9x higher risk if family member has it)
Exercise regularly (may reduce IOP)
Protect eyes from injury
Control diabetes and blood pressure
Avoid steroid eye drops without supervision
Red Flags: When to See a Doctor (AAO)
Seek IMMEDIATE care if experiencing:
- Sudden severe eye pain
- Nausea/vomiting with eye pain
- Sudden blurred vision
- Halos around lights
- Sudden vision loss
Schedule an urgent exam if you:
- Have a family history of glaucoma
- Are over 60 years old
- Notice gradual peripheral vision loss
- Have diabetes or high blood pressure