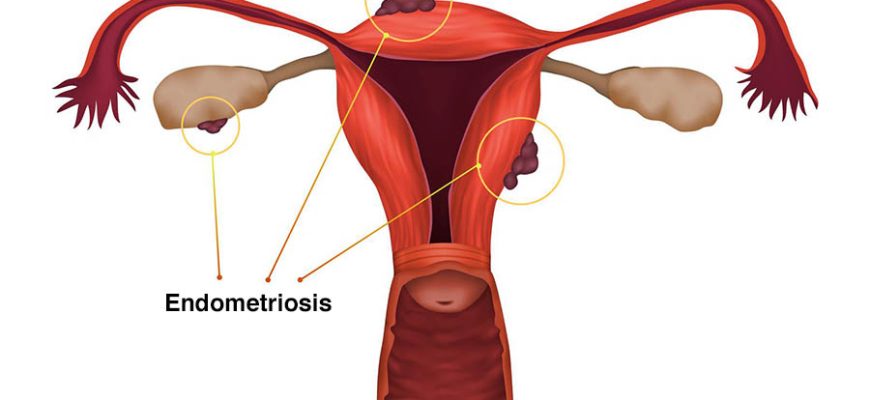
Endometriosis is a chronic, often painful condition where tissue similar to the lining of the uterus (endometrium) grows outside the uterus. This tissue can implant on the ovaries, fallopian tubes, pelvic lining, and other organs, causing inflammation, scarring, and adhesions.
Contents
Causes
The exact cause is unknown, but possible theories include:
- Retrograde menstruation: Menstrual blood flows backward into the pelvis, depositing endometrial cells.
- Immune system dysfunction: The body fails to clear misplaced endometrial cells.
- Hormonal influence: Estrogen promotes the growth of endometrial-like tissue.
- Genetic factors: It tends to run in families.
- Metaplasia: Other cells transform into endometrial-like cells.
Risk Factors
- Family history of endometriosis
- Never giving birth
- Early menarche (first period before age 11)
- Short menstrual cycles (<27 days) or heavy/long periods
- Uterine abnormalities blocking menstrual flow
- Immune disorders
Symptoms
- Pelvic pain (often severe, especially during periods)
- Painful periods (dysmenorrhea)
- Pain during or after sex (dyspareunia)
- Pain with bowel movements or urination (if affecting bladder/bowels)
- Infertility (30-50% of women with endometriosis struggle with fertility)
- Fatigue, bloating, nausea (especially around menstruation)
- Heavy or irregular bleeding
Diagnosis
- Medical history & symptom evaluation
- Pelvic exam (tenderness, nodules)
- Ultrasound (transvaginal or abdominal) – May detect endometriomas (ovarian cysts)
- MRI – Helps map deep endometriosis
- Laparoscopy (gold standard) – Surgical visualization and biopsy for definitive diagnosis
Treatment
1. Pain Management
- NSAIDs (ibuprofen, naproxen) for inflammation
- Hormonal therapies (suppress estrogen-driven growth):
- Birth control pills, patches, or rings
- Progestins (IUDs, injections, pills)
- GnRH agonists (induce temporary menopause)
- Aromatase inhibitors (reduce estrogen production)
2. Surgery
- Laparoscopic excision – Removal of endometrial implants, scar tissue
- Hysterectomy (last resort, removes uterus ± ovaries)
3. Fertility Treatments
- IVF (if natural conception fails)
Prevention
No sure way to prevent endometriosis, but early diagnosis and treatment can slow progression.
- Hormonal birth control may reduce risk
- Exercise and low-fat diet (may lower estrogen levels)
- Avoiding excessive alcohol & caffeine (may influence estrogen)
Complications
- Infertility (due to scarring, inflammation, or ovarian damage)
- Chronic pelvic pain
- Ovarian cysts (endometriomas)
- Bowel/bladder dysfunction (if severe adhesions)
- Increased risk of ovarian cancer & autoimmune diseases
Prognosis
- No cure, but treatments can manage symptoms effectively
- Symptom relief often improves after menopause (unless on HRT)
- Pregnancy may temporarily improve symptoms
- Recurrence is possible, especially after surgery