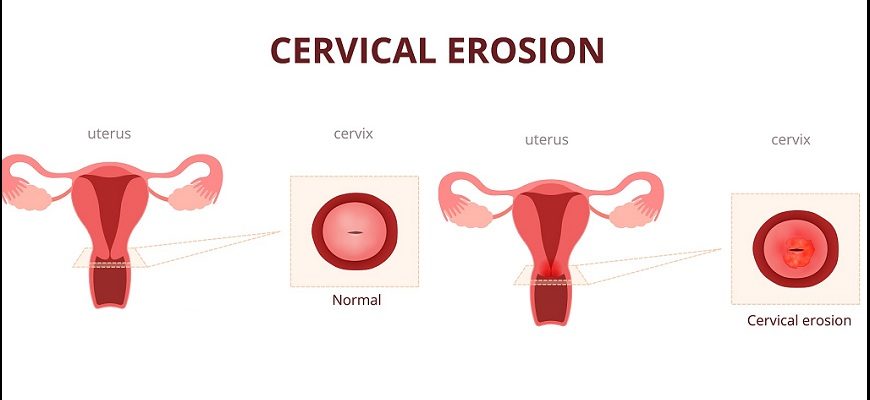
Cervical erosion (medically called cervical ectropion or cervical eversion) is a benign condition where the soft, glandular cells from inside the cervical canal grow outward onto the vaginal portion of the cervix. This makes the cervix appear red and inflamed, though it is not an actual ulcer or wound.
Causes
- Hormonal Changes (Most common)
- Puberty, pregnancy, or birth control pills (estrogen dominance)
- Physical Irritation
- Frequent intercourse, tampon use, or cervical exams
- Congenital (Some women are born with it)
Risk Factors
✔ Young women (common in teens & women in their 20s)
✔ Pregnant women (due to increased estrogen)
✔ Hormonal contraceptive users (pills, patches)
Symptoms
Many women have no symptoms, but some experience:
- Increased vaginal discharge (clear or white, non-foul)
- Spotting/bleeding (after sex, exams, or exercise)
- Mild discomfort (rarely pain)
Note: If discharge is foul-smelling/yellow/green, it may indicate infection (e.g., cervicitis), not just erosion.
Types
- Physiological Ectropion (Normal, hormone-related)
- Traumatic Erosion (From injury, childbirth, or medical procedures)
Diagnosis
- Pelvic Exam – Cervix appears red, inflamed (but smooth, not ulcerated).
- Pap Smear/Colposcopy – Rules out serious conditions (e.g., cervical cancer).
- Infection Testing – If discharge is abnormal (STI screening for chlamydia, gonorrhea).
Treatment
Most cases require NO treatment (resolves on its own).
If symptomatic, options include:
1. Conservative Management
- Monitor & reassure (if no symptoms)
- Treat infections (if present, e.g., antibiotics for cervicitis)
2. Medical Therapy
- Topical estrogen cream (if due to low estrogen post-menopause)
3. Procedural Treatments (Rarely Needed)
- Cryotherapy (freezing affected tissue)
- Silver nitrate cauterization (chemical treatment)
- Electrocautery (LEEP/Diathermy) (for persistent bleeding)
Complications (Rare)
- Recurrent spotting/bleeding (if not treated)
- Increased STI risk (if exposed, due to more fragile tissue)
- Psychological distress (misdiagnosed as STD or cancer)
Prevention
- Avoid unnecessary cervical procedures
- Use lubricants during sex (reduce friction)
- Regular Pap smears (to rule out serious conditions)
Prognosis
- Harmless & often resolves on its own after pregnancy or stopping hormonal birth control.
- Procedures (if needed) are >90% effective in stopping symptoms.
- Does NOT increase cancer risk.
When to See a Doctor?
- Heavy bleeding after sex
- Foul-smelling/yellow discharge (sign of infection)
- Persistent discomfort