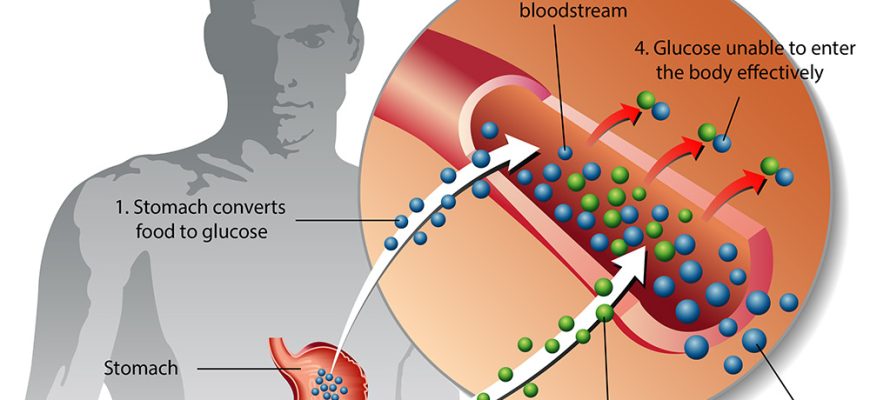
Type 2 diabetes is a chronic metabolic disorder characterized by insulin resistance and relative insulin deficiency, leading to elevated blood glucose
Etiology
Type 2 diabetes involves a complex interplay of genetic, environmental, and lifestyle factors. It is primarily related to:
- Insulin Resistance: The body’s cells become less sensitive to insulin, making it difficult for glucose to enter cells.
- Impaired Insulin Secretion: Over time, the pancreas’ ability to produce sufficient insulin diminishes.
Risk Factors
- Genetics: Family history of diabetes can predispose individuals.
- Obesity: Excess weight, especially around the abdomen, is a significant risk factor.
- Physical Inactivity: Lack of regular exercise contributes to obesity and insulin resistance.
- Age: Risk increases with age, particularly beyond 45 years.
- Ethnicity: Certain groups, including African Americans, Hispanics, Native Americans, and Asian Americans, are at higher risk.
- Gestational Diabetes: Having gestational diabetes during pregnancy also increases the risk of developing type 2 diabetes later.
- Poor diet: Diets high in refined carbohydrates, sugars, and unhealthy fats contribute to obesity and diabetes.
Causes
- Lifestyle Choices: Sedentary lifestyle and poor dietary habits lead to obesity and metabolic changes that precede the onset of diabetes.
- Hormonal Changes: Alterations in hormones, notably those secreted by adipose tissue (like leptin and adiponectin), may play a role in insulin resistance.
Symptoms
- Increased thirst and frequent urination
- Extreme fatigue
- Blurred vision
- Slow-healing wounds or frequent infections
- Areas of darkened skin (acanthosis nigricans)
- Numbness or tingling in hands and feet
Diagnosis
- Fasting Plasma Glucose (FPG): A level of 126 mg/dL (7.0 mmol/L) or higher indicates diabetes.
- Oral Glucose Tolerance Test (OGTT): A 2-hour glucose level of 200 mg/dL (11.1 mmol/L) or higher indicates diabetes.
- Hemoglobin A1C Test: An A1C level of 6.5% or higher indicates diabetes.
- Random plasma glucose testing may also be used if symptoms are present.
Treatment
- Lifestyle Modifications:
- Healthy eating (focused on whole foods, fiber, low saturated fats)
- Regular physical activity (150 minutes of moderate exercise per week)
- Weight loss, if overweight
- Medications: If lifestyle changes are insufficient, medications such as:
- Metformin (first-line treatment)
- Sulfonylureas
- DPP-4 inhibitors
- GLP-1 receptor agonists
- Insulin therapy in some cases
- Monitoring: Regular blood glucose monitoring and periodic A1C checks
Type 2 diabetes requires a multifaceted approach to management. With appropriate interventions, individuals can lead healthy and active lives while minimizing the risk of complications. Regular follow-up with healthcare providers is essential to optimize treatment and monitoring.
Prevention
- Maintain a healthy weight.
- Engage in regular physical activity.
- Eat a balanced diet with whole grains, lean proteins, healthy fats, and plenty of vegetables and fruits.
- Avoid smoking and limit alcohol consumption.
- Regular check-ups, particularly for high-risk individuals.
Complications
- Cardiovascular Disease: Increased risk for heart attacks and strokes.
- Nerve Damage (Neuropathy): Can lead to pain, tingling, and loss of sensation.
- Kidney Damage (Nephropathy): May lead to kidney failure.
- Eye Damage (Retinopathy): Can cause vision loss.
- Foot Damage: Infections and poor healing may lead to amputations.
- Skin Conditions: Infections and various skin disorders are more common.