Sjögren’s syndrome (SS) is a chronic autoimmune disease. In autoimmune diseases, the body’s immune system mistakenly attacks its own healthy tissues. In Sjögren’s, the immune system primarily targets the glands that produce moisture, such as the salivary glands and tear glands. This leads to the hallmark symptoms of dry eyes and dry mouth.
However, it is a systemic disease, meaning it can affect the entire body, including joints, skin, nerves, and internal organs like the lungs, kidneys, and liver.
Causes
The exact cause of Sjögren’s is unknown, but it is believed to be triggered by a combination of genetic and environmental factors.
- Genetic Predisposition: Certain genes make people more susceptible to developing the disease.
- Environmental Trigger: It is hypothesized that a viral or bacterial infection may trigger the immune system to malfunction in genetically susceptible individuals.
- Hormones: The disease is far more common in women (9 out of 10 patients), suggesting hormones may play a role.
Symptoms
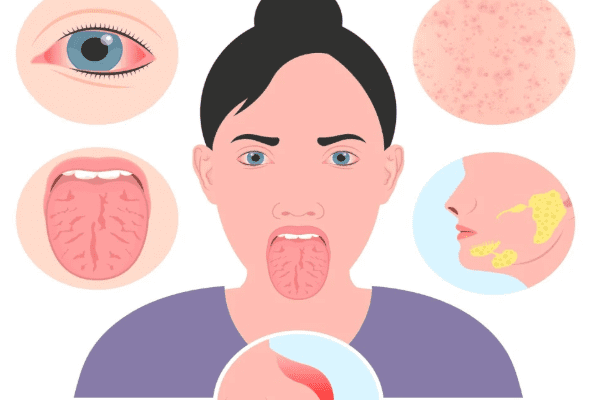
Sjögren’s symptoms can range from mild to debilitating and are divided into two main categories:
1. Glandular Symptoms (Due to lack of moisture):
- Dry Eyes: A gritty, burning, or sandy feeling in the eyes. Itchy eyes and blurred vision.
- Dry Mouth (Xerostomia): Difficulty swallowing, speaking, or tasting. A sticky feeling in the mouth, increased dental cavities, dry cough, and cracked lips.
- Dry Skin and Skin Rashes.
- Vaginal Dryness.
2. Systemic Symptoms (Body-wide):
- Profound Fatigue: This is one of the most common and debilitating symptoms.
- Widespread Joint and Muscle Pain: Similar to that felt in fibromyalgia.
- Brain Fog: Difficulty with concentration and memory.
- Swollen Salivary Glands: Particularly the glands located in front of the ears and under the jaw.
- Other Organ Involvement: Can include dry cough (lung involvement), acid reflux, numbness/tingling in extremities (peripheral neuropathy), and inflammation of organs like the kidneys or thyroid.
Diagnosis
Diagnosing Sjögren’s can be challenging as symptoms mimic other conditions and develop slowly. A rheumatologist typically leads the diagnosis, which may involve:
- Blood Tests:
- Autoantibodies: Testing for specific markers like SSA (Ro) and SSB (La), which are common in Sjögren’s.
- Inflammatory Markers: Checking for elevated ESR and CRP.
- Other Tests: To rule out other conditions and assess organ function.
- Eye Tests:
- Schirmer’s Test: Measures tear production by placing a small paper strip under the eyelid.
- Ocular Staining: An eye doctor uses dyes to check for damage to the surface of the eye caused by dryness.
- Dental/Oral Tests:
- Salivary Flow Test: Measures the amount of saliva produced over a set time.
- Lip Biopsy (The most definitive test): A tiny minor salivary gland is removed from the inside of the lower lip and examined under a microscope for the presence of inflammatory cells characteristic of Sjögren’s.
Treatment
There is no cure for Sjögren’s, so treatment focuses on relieving symptoms and preventing complications.
- Managing Dry Eyes: Artificial tears, lubricating eye gels/ointments, and prescription anti-inflammatory eye drops (e.g., cyclosporine). Punctal plugs can be inserted to block tear drainage.
- Managing Dry Mouth: Sipping water frequently, using artificial saliva, sugar-free lozenges, and prescription medications like pilocarpine or cevimeline that stimulate saliva production. Meticulous dental care is essential.
- Managing Systemic Symptoms:
- Pain and Fatigue: Over-the-counter pain relievers (NSAIDs) and medications like Hydroxychloroquine (Plaquenil) are often used to address joint pain, fatigue, and rashes.
- Organ Involvement: For more severe systemic manifestations, stronger immunosuppressant drugs or biologics (like Rituximab) may be used.
Prevention
There is no known way to prevent Sjögren’s syndrome because the cause is not fully understood. The focus is on early diagnosis and proactive management to prevent complications like dental decay, eye damage, and organ problems.
Prognosis
The prognosis for Sjögren’s is generally good in terms of life expectancy, especially if it is “primary” (occurring alone) and without major organ involvement. However, the quality of life can be significantly impacted by chronic pain, fatigue, and discomfort.
- People with Sjögren’s have a higher risk of developing lymphoma (cancer of the lymph glands) and require regular monitoring.
- With a good management plan, most people can lead full lives, but they must adapt to managing their symptoms daily.
How to Know When to See a Doctor
You should consult your doctor (and ask for a referral to a rheumatologist) if you experience a persistent combination of the following symptoms, especially if they interfere with your daily life:
- Persistent, uncomfortable dryness in the eyes and mouth for more than a few weeks.
- Difficulty chewing, swallowing, or speaking without sipping liquids.
- A sudden increase in dental cavities or mouth sores.
- Swollen salivary glands in your face or neck.
- Unexplained, persistent fatigue that sleep doesn’t resolve.
- Persistent joint pain or muscle aches.
- “Brain fog” that affects your work or daily tasks.
Do not dismiss these symptoms as just “getting older” or “not drinking enough water.” If over-the-counter remedies for dry eyes and mouth aren’t sufficient, it’s time to seek a medical evaluation for a potential underlying autoimmune cause like Sjögren’s syndrome.