What It Is
These are typically characterized by pain, stiffness, swelling, and decreased range of motion in the affected structures.
Causes
There is no single cause for rheumatic diseases, as the category includes over 100 different conditions. Causes can include:
- Autoimmunity: The immune system mistakenly attacks the body’s own tissues (e.g., Rheumatoid Arthritis, Lupus).
- Wear and Tear (Degeneration): Breakdown of cartilage in joints (e.g., Osteoarthritis).
- Inflammation: Systemic inflammation affecting joints and other organs (e.g., Gout, Ankylosing Spondylitis).
- Metabolic Problems: Issues with how the body processes certain substances (e.g., Gout is caused by uric acid crystal buildup).
- Genetics: A family history can increase risk for many rheumatic conditions.
- Environmental Triggers: Infections, smoking, or physical injury may trigger disease in genetically susceptible people.
Symptoms
Symptoms vary greatly depending on the specific disease but often include:
- Pain and stiffness in one or more joints, especially in the morning or after inactivity.
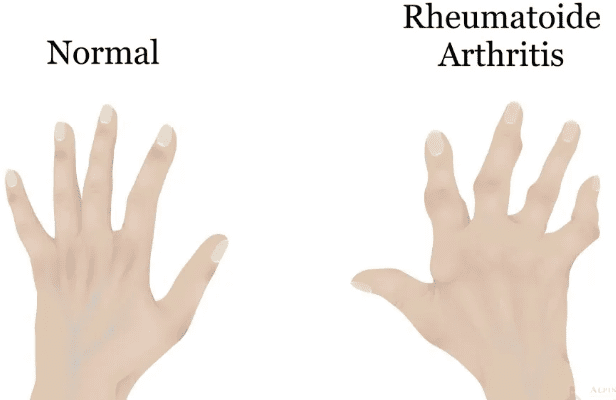
- Swelling, warmth, and redness around the joints.
- Decreased range of motion in a joint.
- Persistent fatigue and a general feeling of being unwell.
- Symptoms that “flare up” and then subside for a period.
Diagnosis
Diagnosing a specific rheumatic disease can be complex and involves several steps:
- Medical History and Physical Exam: A doctor (usually a rheumatologist) will ask about your symptoms, their pattern, and family history, and will examine your joints for swelling, warmth, and tenderness.
- Blood Tests: To check for:
- Inflammatory Markers: ESR (Erythrocyte Sedimentation Rate) and CRP (C-Reactive Protein).
- Autoantibodies: Such as Rheumatoid Factor (RF) and Anti-CCP for RA, or ANA for Lupus.
- Other Markers: Like uric acid for gout.
- Imaging Tests:
- X-rays: To look for joint damage or narrowing of joint space.
- MRI or Ultrasound: Can detect inflammation and early changes not visible on an X-ray.
Treatment
There is no cure for most rheumatic diseases, but effective treatment can control symptoms, prevent joint damage, and maintain quality of life. Treatment is highly personalized and may include:
- Medications:
- Pain Relievers: Acetaminophen or NSAIDs (e.g., Ibuprofen, Naproxen).
- Disease-Modifying Antirheumatic Drugs (DMARDs): Like Methotrexate, to slow disease progression.
- Biologics: Targeted drugs for moderate-to-severe autoimmune forms.
- Corticosteroids: To quickly reduce severe inflammation (e.g., Prednisone).
- Physical and Occupational Therapy: Crucial for maintaining joint function, strength, and learning ways to perform daily tasks with less pain.
- Lifestyle Modifications:
- Regular, low-impact exercise (e.g., swimming, walking).
- Healthy diet to maintain a proper weight and reduce inflammation.
- Heat/Cold Therapy to soothe stiff joints or acute pain.
Prevention
Since “rheumatism” encompasses many conditions with different causes, it cannot be universally prevented. However, you can reduce your risk or delay the onset of some forms (like osteoarthritis) by:
- Maintaining a healthy weight to reduce stress on joints.
- Staying physically active to keep muscles strong and joints flexible.
- Avoiding joint injuries through proper technique during sports and activities.
- Eating a balanced, anti-inflammatory diet.
Prognosis
The prognosis varies dramatically depending on the specific diagnosis, its severity, and how early treatment is started.
- Conditions like osteoarthritis are managed with lifestyle and pain control.
- Inflammatory autoimmune diseases like Rheumatoid Arthritis are chronic but can often be well-controlled with modern medications, allowing people to live full, active lives.
- Early diagnosis and treatment are critical for preventing long-term joint damage and disability.
How to Know When to See a Doctor
You should consult a doctor if you experience any of the following symptoms persistently (for more than a few weeks):
- Pain, swelling, or stiffness in one or more joints that doesn’t go away.
- Joint symptoms that are worse in the morning, characterized by stiffness that lasts for 30 minutes or more.
- Red, warm, or tender joints.
- Persistent fatigue that accompanies joint discomfort.
- Symptoms that make it difficult to perform everyday tasks like climbing stairs, opening jars, or walking.
Do not dismiss persistent joint pain as a normal part of aging. While some wear and tear is common, significant pain, swelling, and morning stiffness are signs of underlying inflammation that warrant a medical evaluation. Start with your primary care physician, who can refer you to a rheumatologist if needed.