Clavicle Fractures: A Comprehensive Guide
What it is:
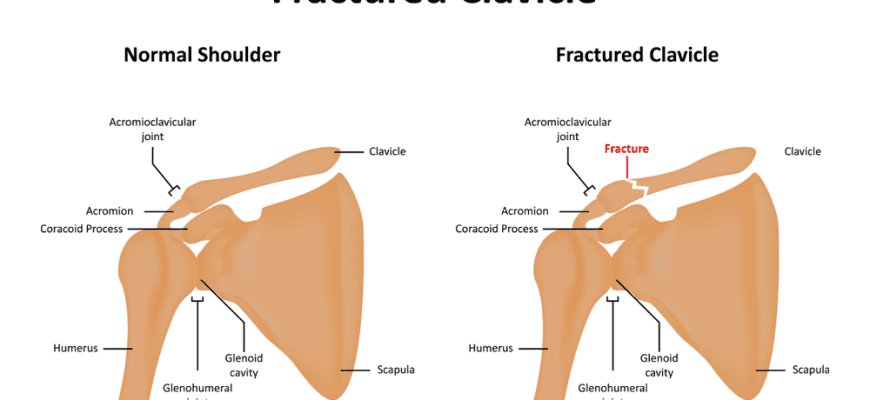
A clavicle fracture, commonly known as a broken collarbone, is a break in the clavicle bone that connects the sternum (breastbone) to the shoulder. It is one of the most common fractures, particularly in children and young adults, and often results from a fall onto the shoulder or an outstretched hand, or direct trauma from contact sports or vehicle accidents.
Types:
Clavicle fractures are classified based on their location along the bone, which influences treatment decisions:
- Group I (Middle Third): The most common type (about 80% of fractures), occurring in the middle portion of the bone. This area is the thinnest and least supported.
- Group II (Distal Third): Occurs near the acromioclavicular (AC) joint, closer to the shoulder. Accounts for about 10-15% of cases. The treatment can be more complex due to the involvement of ligament attachments.
- Group III (Proximal Third): The rarest type (about 5%), occurring near the sternum. These often have a low risk of displacement and are typically treated non-surgically, but require careful monitoring.
Symptoms:
- Immediate sharp pain that worsens with arm movement.
- A visible deformity or “bump” at the fracture site.
- Swelling, bruising, and tenderness over the collarbone.
- A grinding sensation when trying to raise the arm.
- Holding the arm close to the body to support and relieve pain (known as “splinting”).
- In severe cases, the shoulder may appear slumped downward and forward.
Diagnosis:
- Physical Examination: A doctor will check for tenderness, swelling, deformity, and any breaks in the skin. They will also assess neurovascular function (checking pulse and sensation in the arm) to ensure no damage to nerves or blood vessels.
- X-rays: The standard diagnostic tool. They confirm the presence, location, and severity (displacement, comminution/shattering) of the fracture.
- CT Scan: Occasionally used for complex fractures, especially those involving the joints (distal or proximal) to get a more detailed 3D view for surgical planning.
Prevention:
- Use Protective Gear: Wear appropriate, well-fitting pads for contact sports like football, hockey, and lacrosse.
- Practice Safe Habits: Wear a seatbelt in vehicles.
- Maintain Bone Health: Ensure adequate calcium and Vitamin D intake to keep bones strong.
- Strength and Conditioning: Strengthening shoulder, neck, and back muscles can provide better support and stability, though it cannot prevent all injuries from significant trauma.
Treatment:
Treatment depends on the fracture type, displacement, and patient factors (like age and activity level).
- Non-Surgical (Conservative) Treatment: This is the first-line treatment for many fractures, especially non-displaced or minimally displaced ones.
- Arm Sling or Shoulder Immobilizer: Worn for 3-6 weeks to support the arm, align the bone, and manage pain.
- Medication: Over-the-counter NSAIDs (e.g., ibuprofen) or acetaminophen for pain.
- Physical Therapy: Once initial healing begins (around 4-6 weeks), therapy is crucial to restore range of motion, strength, and function.
- Surgical Treatment: Surgery is recommended for:
- Fractures with significant displacement (the bone ends are far apart).
- “Comminuted” fractures (bone is broken into several pieces).
- Fractures that have broken through the skin (open fracture).
- Fractures threatening the skin (tenting).
- Fractures with associated neurovascular injury.
- Cases where non-surgical treatment has failed (nonunion).
Types of Surgeries:
- Open Reduction and Internal Fixation (ORIF): This is the most common procedure.
- Plates and Screws: A metal plate is contoured to the bone and secured with screws to hold the fragments in place while they heal. This is the most robust fixation.
- Intramedullary Fixation: A metal pin is inserted down the center (canal) of the bone to stabilize the fracture. It is less invasive but may be less stable for complex fractures and often requires a second surgery for removal.
Prognosis:
The prognosis for a clavicle fracture is generally very good.
- Non-Surgical: Most fractures heal well with a sling. The main risks are a visible bump (from healing in a slightly displaced position) and a slightly shorter clavicle length, which rarely affects function for everyday activities.
- Surgical: Surgery aims to restore normal anatomy, which can lead to a higher rate of union and potentially better strength for high-demand athletes. Recovery involves 6-8 weeks of restricted activity followed by physical therapy. Most patients return to full activity within 3-4 months.
- Potential Complications: Include nonunion (failure to heal), malunion (healing in a bad position), hardware irritation (the plate feeling prominent under the skin), and, rarely, infection or nerve injury.
Warning Signs & When to See a Doctor:
Seek immediate medical attention at an urgent care clinic or emergency room after any significant trauma if you suspect a broken bone.
Go to the Emergency Room immediately if you experience:
- Numbness, tingling, or a “pins and needles” feeling in the arm or hand.
- The arm or hand feels cold or turns blue or white.
- A visible break in the skin where the bone may be protruding (open fracture).
These are signs of potential nerve or blood vessel damage and require urgent evaluat