Fractures of the Hand: A Comprehensive Guide
What it is:
A hand fracture is a break in any of the 27 bones in the hand. This includes the bones in the palm (metacarpals) and the bones in the fingers (phalanges). They are extremely common injuries, accounting for nearly one-third of all fractures treated in the emergency room. Proper treatment is critical to restore the hand’s complex function, which involves precise motion, grip strength, and sensitivity.
Types:
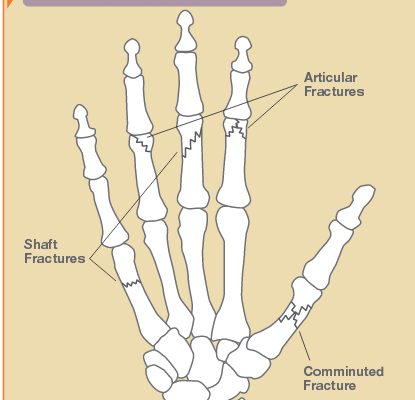
Hand fractures are classified by the specific bone and location of the break:
- Metacarpal Fractures: Breaks in the long bones of the palm that connect the wrist to the fingers.
- Boxer’s Fracture: A specific fracture of the “neck” of the 5th metacarpal (the bone leading to the pinky finger), often from punching a hard object.
- Bennett’s Fracture: A fracture at the base of the 1st metacarpal (thumb bone) that extends into the carpometacarpal (CMC) joint. It is unstable and often requires surgery.
- Phalangeal Fractures: Breaks in the bones of the fingers (phalanges). These can occur at the base, shaft, or tip of the finger and can involve the joints.
- Intra-articular vs. Extra-articular: This critical distinction refers to whether the fracture line extends into a joint surface. Intra-articular fractures are more serious as they can lead to post-traumatic arthritis if not aligned perfectly.
- Open vs. Closed: An open (compound) fracture means the bone has broken through the skin, creating a risk of infection.
Symptoms:
- Immediate, sharp pain at the site of the break, worsened by any movement or grip.
- Significant swelling and bruising.
- Tenderness to touch directly over the fractured bone.
- Visible deformity, such as a finger that is misaligned, shortened, or rotated.
- Inability to move the finger or make a fist without severe pain.
- In some cases, numbness or tingling (a sign of potential nerve injury).
Diagnosis:
- Physical Examination: A doctor will look for swelling, deformity, and open wounds. They will assess rotational alignment (asking you to make a fist to see if the fingers align properly) and check for nerve and blood vessel function.
- X-rays: The primary diagnostic tool. At least two different views (anteroposterior and oblique) are taken to visualize the fracture’s location, displacement, and alignment. Stress views may be used for certain ligamentous injuries.
Prevention:
- Use Protective Gear: Wear appropriate gloves and padding for work (e.g., construction) and sports (e.g., football, basketball).
- Fall Prevention: Practice safety measures to avoid falls, especially for older adults with osteoporosis.
- Proper Technique: Use correct form in sports and weightlifting to avoid undue stress on the hands.
Treatment:
The goal is to heal the bone in a position that allows for full function.
- Non-Surgical Treatment: Used for stable, non-displaced, or minimally displaced fractures.
- Splinting or Casting: A cast or specialized splint (e.g., ulnar gutter splint) is used to immobilize the fracture for 3-6 weeks.
- Buddy Taping: Taping an injured finger to a healthy neighboring one for support and protection.
- Closed Reduction: For some displaced fractures, a doctor can manually realign the bones under local anesthesia before applying a splint.
- Surgical Treatment: Required for unstable fractures that cannot be held in place with a cast.
- Indications: Significant displacement, rotational deformity, multiple fractures, open fractures, and intra-articular fractures involving the joint surface.
Types of Surgeries:
- Open Reduction and Internal Fixation (ORIF): The most common procedure.
- Kirschner Wires (K-wires): Thin metal pins that are inserted through the skin to hold bone fragments in place. They are often temporary and removed after healing.
- Screws: Used alone for large, discrete fragments.
- Plates and Screws: Small metal plates are applied to the bone to hold multiple fragments in precise anatomical alignment. This allows for earlier motion.
- External Fixation: Used for severe open fractures with significant bone loss or soft tissue damage. A frame outside the body holds the bones in place with pins.
Prognosis:
- Non-Surgical: Most non-displaced hand fractures heal well with immobilization, followed by hand therapy. Stiffness is common but usually resolves.
- Surgical: With modern techniques, outcomes are generally very good. The key to a successful outcome is early controlled motion after surgery, guided by a hand therapist, to prevent permanent stiffness.
- Potential Complications: Include stiffness (most common), malunion (healing in a poor position), nonunion (failure to heal), infection, and post-traumatic arthritis.
Warning Signs & When to See a Doctor:
You should see a doctor (an orthopedic urgent care or ER) for any significant hand injury that causes pain, swelling, and difficulty moving the fingers.
Go to the Emergency Room immediately if you experience:
- Numbness or tingling in the fingertips (sign of nerve injury).
- Fingertips that are pale, cold, or blue (sign of vascular injury).
- An open wound where the bone may be protruding.
- A finger that is severely deformed, rotated, or bent.
- Inability to actively straighten a finger (may indicate a tendon injury).