Bechterev’s Disease: A Comprehensive Guide (Ankylosing Spondylitis)
What It Is
Bechterev’s disease is more commonly known in the U.S. as Ankylosing Spondylitis (AS). It is a chronic, inflammatory autoimmune disease that primarily affects the axial skeleton, meaning the spine and sacroiliac joints (where the base of the spine connects to the pelvis). Over time, the inflammation can lead to the fusion of vertebrae, a process called ankylosis, which can cause the spine to become rigid and inflexible. It is a systemic condition, meaning it can affect other parts of the body, including the eyes, heart, lungs, and intestines.
Types
While Ankylosing Spondylitis is the primary term, it falls under a larger category of diseases called Spondyloarthropathies. Related types include:
- Non-Radiographic Axial Spondyloarthritis (nr-axSpA): Inflammation and symptoms are present, but definitive damage is not yet visible on X-rays.
- Peripheral Spondyloarthritis: Inflammation affects joints outside the spine, such as the arms and legs (knees, ankles, etc.).
- Enteropathic Arthritis: Spondyloarthritis associated with Inflammatory Bowel Disease (IBD) like Crohn’s disease or ulcerative colitis.
- Psoriatic Arthritis: Spondyloarthritis associated with the skin condition psoriasis.
- Reactive Arthritis: Spondyloarthritis triggered by an infection elsewhere in the body.
Symptoms
Symptoms often start in early adulthood and can vary in severity.
- Early and Primary Symptoms:
- Chronic pain and stiffness: In the lower back, buttocks, and hips, which develops gradually over weeks or months.
- Pain that improves with activity and worsens with rest: This is a hallmark sign, distinguishing it from mechanical back pain.
- Morning stiffness: Lasting for 30 minutes or longer.
- Pain that wakes you up: In the second half of the night due to inflammation.
- Advanced Symptoms:
- Loss of spinal flexibility: Inability to bend or twist the spine.
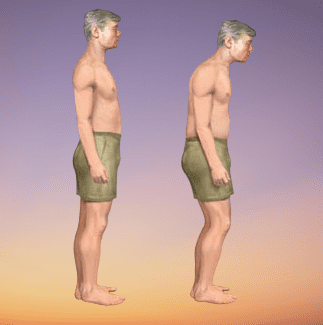
- Stooped posture (Kyphosis): As vertebrae fuse, a forward-curving posture can develop.
- Pain in other joints: Such as the hips, knees, shoulders, and ribs.
- Enthesitis: Pain where tendons and ligaments attach to bone (e.g., Achilles tendon, bottom of the foot).
- Systemic Symptoms:
- Fatigue: A common and significant symptom.
- Uveitis (Iritis): A painful, red, inflamed eye that is a medical emergency and requires prompt treatment to prevent vision loss.
- Inflammatory Bowel Disease (IBD).
- Psoriasis.
- Rarely, heart and lung involvement.
Diagnosis
Diagnosis can be challenging as early signs may not show on X-rays. It involves:
- Medical History and Physical Exam: A doctor (rheumatologist) will assess pain patterns, morning stiffness, and family history. They may measure chest expansion and spinal mobility.
- Imaging:
- X-rays: To look for changes and fusion in the sacroiliac joints and spine. Changes may take years to appear.
- MRI (Magnetic Resonance Imaging): Can detect early inflammation (sacroiliitis) and edema in the bones before damage is visible on X-ray. This is key for diagnosing non-radiographic axial SpA.
- Blood Tests:
- HLA-B27 Gene Test: Most people with AS test positive for this genetic marker. However, having the gene does not mean you will get the disease, and some people with AS test negative.
- Inflammation Markers: ESR (erythrocyte sedimentation rate) and CRP (C-reactive protein) may be elevated, but not always.
Prevention
There is no known way to prevent Ankylosing Spondylitis as its cause is believed to be genetic and autoimmune. However, the goal is to prevent progression, disability, and complications through early diagnosis and consistent treatment.
Treatment
Treatment focuses on relieving pain, reducing inflammation, maintaining posture, and preventing deformity.
- Physical Therapy and Exercise: This is the cornerstone of treatment. Daily exercises and physiotherapy are crucial to maintain flexibility, posture, and range of motion.
- Medications:
- NSAIDs: Nonsteroidal anti-inflammatory drugs (e.g., Naproxen, Ibuprofen) are first-line treatment to reduce pain and inflammation.
- DMARDs: Disease-Modifying Antirheumatic Drugs (e.g., Sulfasalazine) can help with peripheral joint pain but are less effective for spinal symptoms.
- Biologics (TNF inhibitors and IL-17 inhibitors): These are highly effective for many patients. They target specific parts of the immune system to control inflammation and can halt disease progression. Examples include adalimumab (Humira), secukinumab (Cosentyx), and ixekizumab (Taltz).
- Corticosteroid Injections: Can be used for short-term relief in inflamed joints.
Types of Surgery
Surgery is rare and reserved for severe cases where joint damage is crippling.
- Joint Replacement: Hip replacement (arthroplasty) is the most common surgery for AS, performed if the hip joints are severely damaged and painful.
- Spinal Osteotomy: A procedure where a wedge is cut out of a fused section of the spine to correct severe, disabling kyphosis (hunchback posture). It carries significant risk.
- Spinal Fusion Surgery: To stabilize the neck or correct instability in the spine.
Prognosis
The course of AS is highly variable and unpredictable. It is a lifelong condition, but it is not crippling for most people.
- With modern treatments, particularly biologics, most patients can lead full, productive lives.
- Disease activity often becomes less aggressive after middle age.
- The prognosis is best with an early diagnosis and a proactive treatment plan that includes medication and daily exercise.
- Severe cases can lead to significant spinal fusion and disability.
Warning Signs & When to See a Doctor
You should see a rheumatologist if you experience:
- Persistent lower back pain and stiffness that started before age 40.
- Back pain that improves with exercise and worsens with rest.
- Morning stiffness that lasts more than 30 minutes.
- Pain in your buttocks that alternates from one side to the other.
- Unexplained pain in other joints or tendons (heels, chest).
- Associated symptoms like recurrent eye inflammation (red, painful eye), psoriasis, or IBD.