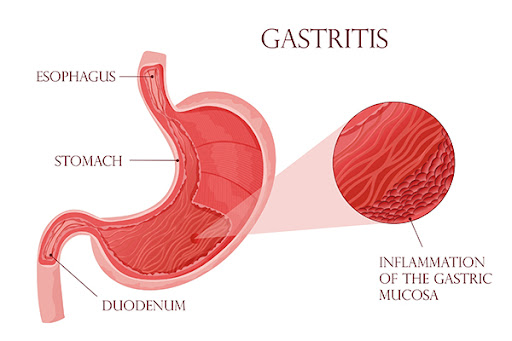
Gastritis is the inflammation of the stomach lining. It can be classified as acute or chronic and can result from various causes.
Contents
Etiology
- Infectious Agents:
- Helicobacter pylori: A common bacterium that can cause chronic gastritis.
- Other infections, including viral (e.g., cytomegalovirus) or fungal infections in immunocompromised individuals.
- Chemical Irritants:
- Nonsteroidal anti-inflammatory drugs (NSAIDs).
- Alcohol consumption.
- Bile reflux (when bile flows back into the stomach).
- Autoimmune Reactions:
- Autoimmune gastritis occurs when the immune system attacks the stomach lining.
- Stress:
- Physical stress, such as severe illness, surgery, or injury, can lead to acute gastritis.
- Dietary Factors:
- Spicy food, certain food intolerances, and allergies may contribute to gastritis.
Risks and Causes
- Age: Older adults are at higher risk due to a greater likelihood of existing medical issues.
- H. pylori Infection: A major cause of chronic gastritis.
- Medications: Long-term NSAID use, corticosteroids, and other drugs that irritate the stomach lining.
- Alcohol Abuse: Chronic ingestion of alcohol is a major risk factor.
- Autoimmune Diseases: Conditions that increase the risk of autoimmune gastritis.
Types of Gastritis
- Acute Gastritis: Sudden onset of inflammation, often due to irritants like NSAIDs or alcohol.
- Chronic Gastritis: Long-term inflammation that may result from persistent H. pylori infection or autoimmune conditions:
- Type A Gastritis: Autoimmune gastritis affecting the body’s ability to produce intrinsic factor.
- Type B Gastritis: More common, often linked to H. pylori infection.
- Atrophic Gastritis: Characterized by the thinning of the stomach lining, which can lead to vitamin B12 deficiency and increase the risk of stomach cancer.
Symptoms
- Abdominal pain or discomfort.
- Nausea or vomiting.
- Bloating and a feeling of fullness.
- Loss of appetite.
- Indigestion or dyspepsia.
- In severe cases, gastrointestinal bleeding (e.g., vomit that looks like coffee grounds or black stools).
Diagnosis
- Medical History and Physical Examination: Understanding symptoms and lifestyle factors.
- Endoscopy: Allows direct visualization of the stomach lining and facilitates biopsies if necessary.
- Biopsy: To check for H. pylori infection or other pathological changes in the tissue.
- Lab Tests: Blood tests to assess for anemia, inflammation, and H. pylori infection (via stool antigen tests or urea breath tests).
Treatment
- Medications:
- Proton Pump Inhibitors (PPIs): Reduce stomach acid and promote healing.
- H2-Receptor Antagonists: Reduce acid production.
- Antacids: Provide symptomatic relief.
- Antibiotics: If H. pylori is present.
- Corticosteroids: For autoimmune-related gastritis.
- Dietary Modifications: Avoid irritative foods and beverages (e.g., spicy foods, alcohol, caffeine).
- Lifestyle Changes: Reducing stress, quitting smoking, and moderating alcohol intake.
Prevention
- Proper hygiene to prevent bacterial infections.
- Limiting the use of NSAIDs and alcohol.
- Eating a balanced diet that avoids known irritants.
- Stress management techniques.
Complications
- Peptic Ulcers: Open sores in the stomach lining or upper part of the small intestine.
- Stomach Bleeding: This can lead to anemia.
- Stomach Cancer: Long-term inflammation associated with chronic gastritis may increase the risk.
- Vitamin Deficiencies: Especially in cases of atrophic gastritis leading to malabsorption of nutrients.