Osteoarthritis of the Spine: A Comprehensive Guide
What it is:
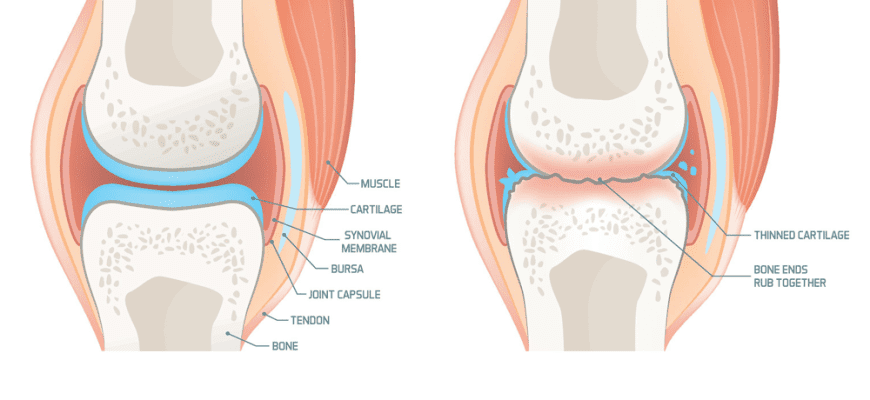
Osteoarthritis (OA) of the spine, also commonly called spinal arthritis or facet joint arthritis, is a degenerative “wear-and-tear” condition that affects the joints of the spine. Unlike osteochondrosis, which primarily targets the discs, OA specifically involves the breakdown of the protective cartilage that cushions the ends of the bones in the facet joints—the small joints located between and behind vertebrae that allow for spinal movement. As the cartilage wears down, bone rubs on bone, leading to pain, inflammation, and the development of bone spurs (osteophytes).
Types:
While OA is a general condition, it’s categorized by the region of the spine it affects:
- Cervical Osteoarthritis (Cervical Spondylosis): Affects the facet joints in the neck. It is extremely common with aging.
- Lumbar Osteoarthritis: Affects the facet joints in the lower back. This is also very common due to the high loads the lower back carries.
- Thoracic Osteoarthritis: Affects the mid-back. This is less common because the thoracic spine is more rigid and stable due to its connection to the rib cage.
Symptoms:
Symptoms can vary from mild to severe and often worsen as the day progresses or after activity.
- Localized pain: A deep, aching pain in the affected region of the neck or back. It is often described as a “bone-on-bone” feeling.
- Stiffness: Most noticeable upon waking up in the morning or after a period of inactivity.
- Tenderness: The area over the affected joint may be sore to the touch.
- Grating sensation: A feeling of grinding or popping (crepitus) with movement.
- Bone spurs: These can compress nearby nerves, leading to radiculopathy.
- Radiculopathy: If nerve roots are compressed, pain, numbness, tingling, or weakness can radiate into the shoulders, arms, hands (from cervical OA) or buttocks, hips, legs (from lumbar OA). This is often called a “pinched nerve.”
Diagnosis:
Diagnosis involves a combination of methods:
- Medical History and Physical Exam: A doctor will discuss your symptoms, assess your range of motion, check for pain with movement or tenderness, and test reflexes and muscle strength to identify nerve involvement.
- Imaging Tests:
- X-rays: Can show the loss of cartilage (indicated by narrowed joint space), bone spurs, and other bony changes.
- Magnetic Resonance Imaging (MRI): Provides detailed images of soft tissues, including nerves and discs, to assess if nerve compression is causing radiculopathy.
- Computed Tomography (CT) Scan: Useful for seeing detailed bone anatomy.
- Diagnostic Injections (Nerve Blocks): Injecting a local anesthetic into a specific facet joint. If the pain is temporarily relieved, it confirms that joint as the source of pain.
Prevention:
You cannot prevent all arthritis, but you can slow its progression and reduce symptoms.
- Maintain a Healthy Weight: Reduces stress on the spine’s joints.
- Stay Active: Regular, low-impact exercise strengthens the core and back muscles, which act as a natural brace for the spine.
- Practice Good Posture: Reduces uneven pressure on the facet joints.
- Use Proper Lifting Techniques: Lift with your legs, not your back.
- Avoid Smoking: Smoking accelerates disc degeneration, which can exacerbate spinal instability and arthritis.
Treatment:
There is no cure for OA, so treatment focuses on managing pain and improving function.
- Lifestyle Modifications: Weight loss, activity modification to avoid painful movements.
- Physical Therapy: The cornerstone of treatment. A physical therapist designs exercises to improve flexibility, strengthen core muscles, and correct posture.
- Medications:
- Over-the-counter (OTC): Acetaminophen (Tylenol), NSAIDs (ibuprofen, naproxen).
- Prescription: Stronger anti-inflammatories, topical pain creams, or muscle relaxants.
- Injections:
- Corticosteroid Injections: Powerful anti-inflammatory injections directly into the facet joint or around a nerve to provide weeks or months of pain relief.
- Radiofrequency Ablation (RFA): A procedure that uses heat to disable the nerves carrying pain signals from the arthritic joint. This can provide longer-term relief (6 months to 2 years).
Types of Surgery:
Surgery is a last resort when extensive conservative treatment fails and there is severe nerve compression or spinal instability.
- Laminectomy: Removal of the lamina (part of the vertebra) to create more space for nerves, relieving pressure caused by bone spurs and stenosis.
- Discectomy: Removal of a portion of a herniated disc that is contributing to nerve compression.
- Spinal Fusion: Permanently connecting two or more vertebrae together with bone grafts and hardware (screws/rods) to stop motion at a painful arthritic joint. This is the most common surgery for severe spinal OA.
- Artificial Disc Replacement (ADR): A less common alternative to fusion for certain patients, where a damaged disc is replaced with an artificial device to preserve motion.
Prognosis:
Osteoarthritis is a chronic, progressive condition. However, the prognosis for most people is good. With a consistent management plan involving physical therapy and lifestyle changes, most people can effectively control their pain, remain active, and maintain a good quality of life. It does not typically lead to serious disability.
Warning Signs & When to See a Doctor:
Consult a doctor if you experience:
- Persistent back or neck pain that doesn’t improve with rest and OTC medication after a week or two.
- Pain that radiates into your arms or legs.
- Numbness, tingling, or weakness in your limbs.
- Loss of bowel or bladder control. This is a sign of cauda equina syndrome, a medical emergency that requires immediate attention.
- Significant, unexplained weight loss accompanied by back pain (to rule out other causes).