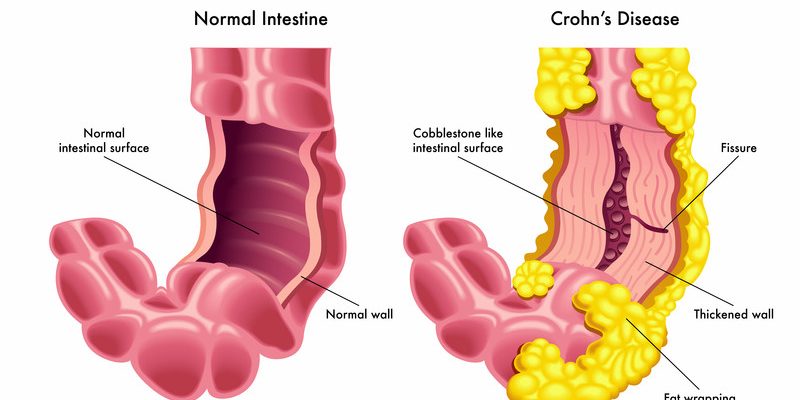
Crohn’s disease is a chronic inflammatory bowel disease (IBD) that causes digestive tract inflammation, most commonly affecting the small intestine and colon. It is characterized by flare-ups (active symptoms) and remission (symptom-free periods). Unlike ulcerative colitis, Crohn’s can affect any part of the GI tract, from mouth to anus, in patchy, deep inflammation.
Etiology (Causes & Risk Factors)
The exact cause is unknown, but research suggests:
✔ Genetic factors – Mutations in *NOD2/CARD15* gene (15% of cases have a family history)
✔ Immune system dysfunction – Overactive immune response attacks gut bacteria
✔ Environmental triggers – Smoking, diet (processed foods), antibiotics, NSAIDs
✔ Microbiome imbalance – Reduced gut bacteria diversity
✔ Ethnicity & geography – More common in Western countries, Ashkenazi Jews
Types of Crohn’s Disease
- Ileocolitis (most common) – Affects ileum + colon
- Ileitis – Only small intestine (ileum)
- Gastroduodenal Crohn’s – Stomach + duodenum
- Jejunoileitis – Upper small intestine (jejunum)
- Crohn’s (granulomatous) colitis – Colon only
- Perianal Crohn’s – Fistulas, abscesses near anus
Symptoms
Common Symptoms
- Diarrhea (chronic, sometimes bloody)
- Abdominal pain & cramping (often lower right side)
- Weight loss & malnutrition (due to poor nutrient absorption)
- Fatigue & fever (from inflammation)
- Mouth sores & reduced appetite
Complications
- Strictures (narrowed intestines → blockages)
- Fistulas (abnormal tunnels between organs)
- Abscesses (infected pus pockets)
- Colon cancer (long-term risk)
- Arthritis, skin rashes, eye inflammation (extra-intestinal effects)
Diagnosis
No single test confirms Crohn’s—diagnosis involves:
- Colonoscopy + biopsy (gold standard, checks inflammation patterns)
- Blood tests (anemia, high CRP/ESR = inflammation)
- Stool tests (rule out infections like C. difficile)
- Imaging (MRI/CT enterography, capsule endoscopy)
- Balloon-assisted enteroscopy (for small intestine evaluation)
Treatment
1. Medications
- Anti-inflammatories (mesalamine, corticosteroids)
- Immunosuppressants (azathioprine, methotrexate)
- Biologics (anti-TNF like infliximab, ustekinumab)
- Antibiotics (for infections, fistulas)
2. Surgery (needed in 70% of cases)
- Strictureplasty (widens narrowed intestines)
- Bowel resection (removes damaged sections)
- Fistula repair
3. Lifestyle & Diet
- Low-residue diet (during flares)
- Vitamin supplements (B12, iron, D)
- Stress management (yoga, therapy)
Prevention (Reducing Flares)
While Crohn’s can’t be fully prevented, these help:
✔ Quit smoking (doubles flare risk)
✔ Avoid NSAIDs (worsen inflammation)
✔ Probiotics & fiber (during remission)
✔ Regular check-ups (monitor inflammation)
When to See a Doctor
Emergency signs:
- Severe abdominal pain + vomiting (possible blockage)
- High fever + bloody diarrhea
- Sudden weight loss (10+ lbs unintentionally)
Early warning signs:
- Persistent diarrhea (2+ weeks)
- Unexplained joint pain or rashes
- Family history of IBD
How to Avoid Complications
- Stick to treatment (even in remission)
- Get colonoscopies (monitor for cancer)
- Hydrate + eat small meals (reduce bowel stress)
- Exercise (improves gut motility)
Final Note:
Crohn’s is lifelong but manageable with modern therapies. Early diagnosis prevents severe damage. If you suspect symptoms, see a gastroenterologist.