Contents
- Etiology & Causes
- 1. Genetic Factors:
- 2. Immune Dysregulation:
- 3. Environmental Triggers:
- Symptoms
- Acute Phase:
- Chronic Phase:
- Age-Specific Patterns:
- Diagnosis
- Prevention
- 1. Skin Barrier Protection:
- 2. Trigger Avoidance:
- 3. Dietary (Controversial):
- Treatment
- 1. Topical Therapies:
- 2. Systemic Therapies (Moderate-Severe AD):
- 3. Adjunctive Care:
- When to See a Doctor (Red Flags)
- Key Takeaways
- Key Differences: Atopic Dermatitis vs. Exanthem
- 1. Definition & Nature
- 2. Causes & Triggers
- 3. Symptoms
- 4. Duration & Course
- 5. Diagnosis
- 6. Treatment
- 7. When to Worry
- Summary Table
Etiology & Causes
AD results from a complex interplay of genetic, immune, and environmental factors:
1. Genetic Factors:
- Mutations in filaggrin (FLG) gene (impairs skin barrier function).
- Family history of atopy (eczema, asthma, allergies).
2. Immune Dysregulation:
- Th2-dominant immune response → Excess IgE and cytokines (IL-4, IL-13).
- Skin microbiome imbalance (↑ Staphylococcus aureus).
3. Environmental Triggers:
- Allergens: Dust mites, pet dander, pollen.
- Irritants: Harsh soaps, detergents, fragrances.
- Climate: Low humidity, extreme temperatures.
- Stress & Hormones: Flare-ups during stress/pregnancy.
Symptoms
Acute Phase:
- Intense itching (pruritus), worse at night.
- Red, swollen patches with small blisters (may ooze).
- Common sites: face (infants), flexural areas (elbows, knees).
Chronic Phase:
- Lichenification (thickened, leathery skin).
- Dry, scaly patches with cracks/fissures.
- Secondary infections (yellow crusts = bacterial; vesicles = viral).
Age-Specific Patterns:
- Infants (0–2 yrs): Cheeks, scalp, extensor surfaces.
- Children (>2 yrs): Neck, wrists, ankles, flexural creases.
- Adults: Hands, eyelids, severe lichenification.
Diagnosis
- Clinical Criteria (Hanifin & Rajka):
- Major: Pruritus, typical morphology/distribution, chronic relapsing course.
- Minor: Dry skin, early age onset, personal/family atopy, IgE reactivity.
- Tests (if needed):
- Patch testing (rule out contact dermatitis).
- Skin biopsy (rare, to exclude psoriasis/t-cell lymphoma).
- Blood tests: Elevated IgE (not required for diagnosis).
Prevention
1. Skin Barrier Protection:
- Daily emollients (ceramide-based creams, e.g., CeraVe).
- Lukewarm baths + immediate moisturizing (“soak and seal”).
2. Trigger Avoidance:
- Fragrance-free, hypoallergenic products.
- Cotton clothing, avoid wool/synthetics.
- Humidifiers in dry climates.
3. Dietary (Controversial):
- For infants with severe AD, consider eliminating cow’s milk/eggs (under doctor supervision).
Treatment
1. Topical Therapies:
- Steroids (hydrocortisone, betamethasone): Short-term for flares.
- Calcineurin inhibitors (tacrolimus, pimecrolimus): Steroid-free for face/sensitive areas.
- PDE4 inhibitors (crisaborole): Anti-inflammatory ointment.
2. Systemic Therapies (Moderate-Severe AD):
- Oral antihistamines (e.g., cetirizine) for itching.
- Dupilumab (biologic): Targets IL-4/IL-13 (for refractory cases).
- JAK inhibitors (upadacitinib): Rapid itch relief.
3. Adjunctive Care:
- Wet wrap therapy (for severe flares).
- Bleach baths (diluted, for infected AD).
When to See a Doctor (Red Flags)
Seek immediate care if:
- Worsening rash despite treatment.
- Signs of infection (pus, fever, painful sores → may need antibiotics).
- Eye involvement (redness/itching → risk of keratoconus).
- Sleep disruption or mental health impact (chronic itching → anxiety/depression).
Emergency:
- Eczema herpeticum (clustered blisters + fever → HSV infection).
Key Takeaways
- AD is chronic but manageable with barrier repair + trigger avoidance.
- Topical steroids are first-line; biologics help severe cases.
- Early intervention prevents complications (infections, scarring).
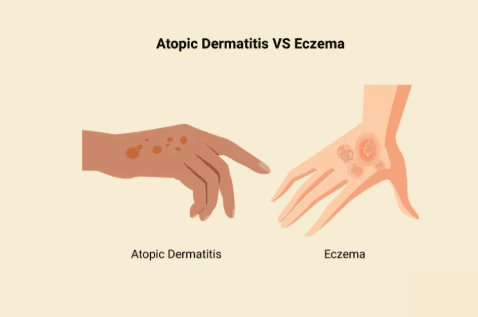
Key Differences: Atopic Dermatitis vs. Exanthem
1. Definition & Nature
| Atopic Dermatitis (AD) | Exanthem |
|---|---|
| Chronic, relapsing inflammatory skin disease linked to skin barrier dysfunction and immune dysregulation (Th2 dominance). | Acute, widespread rash (often viral/bacterial/drug-induced). |
| Type of eczema; part of the “atopic triad” (asthma, allergies). | Symptom of systemic illness (e.g., measles, scarlet fever, drug reactions). |
2. Causes & Triggers
| Atopic Dermatitis | Exanthem |
|---|---|
| – Genetic (filaggrin mutations) – Environmental allergens (dust mites, pollen) – Skin irritants (soaps, fabrics) – Stress | – Infections (viruses: measles, HHV-6; bacteria: strep) – Drug reactions (antibiotics, anticonvulsants) – Autoimmune (Kawasaki disease) |
3. Symptoms
| Atopic Dermatitis | Exanthem |
|---|---|
| – Itchy, dry, scaly patches – Lichenification (thickened skin) in chronic cases – Flexural areas (elbows/knees), face (infants) | – Sudden rash (maculopapular, vesicular, etc.) – Often accompanies fever/malaise – Trunk/limbs symmetrically affected |
4. Duration & Course
| Atopic Dermatitis | Exanthem |
|---|---|
| Chronic (flare-ups and remissions) | Acute (resolves in days–weeks with treatment) |
5. Diagnosis
| Atopic Dermatitis | Exanthem |
|---|---|
| – Clinical history + exam (Hanifin & Rajka criteria) – Elevated IgE (sometimes) – Patch testing (if contact allergy suspected) | – Identify underlying cause (viral titers, throat swab for strep) – Drug history – May need skin biopsy |
6. Treatment
| Atopic Dermatitis | Exanthem |
|---|---|
| – Emollients (ceramide creams) – Topical steroids/calcineurin inhibitors – Dupilumab (biologic for severe cases) | – Treat underlying cause (antivirals, antibiotics) – Symptomatic relief (antihistamines, antipyretics) – Discontinue offending drug |
7. When to Worry
| Atopic Dermatitis | Exanthem |
|---|---|
| – Bacterial infection (oozing, pus) – Eczema herpeticum (HSV blisters + fever) | – Stevens-Johnson syndrome (blisters + mucosal involvement) – High fever + petechiae (meningococcemia risk) |
Summary Table
| Feature | Atopic Dermatitis | Exanthem |
|---|---|---|
| Duration | Chronic | Acute |
| Itching | Severe | Mild/absent |
| Fever | Rare | Common |
| Distribution | Flexural/face | Widespread |
| Cause | Genetic + environmental | Infection/drugs |
Bottom Line:
- Atopic dermatitis is chronic, itchy, and localized (eczema).
- Exanthem is acute, often febrile, and systemic (rash + infection/drugs).