Dislocations of the Wrist and Fingers: A Comprehensive Guide
What it is:
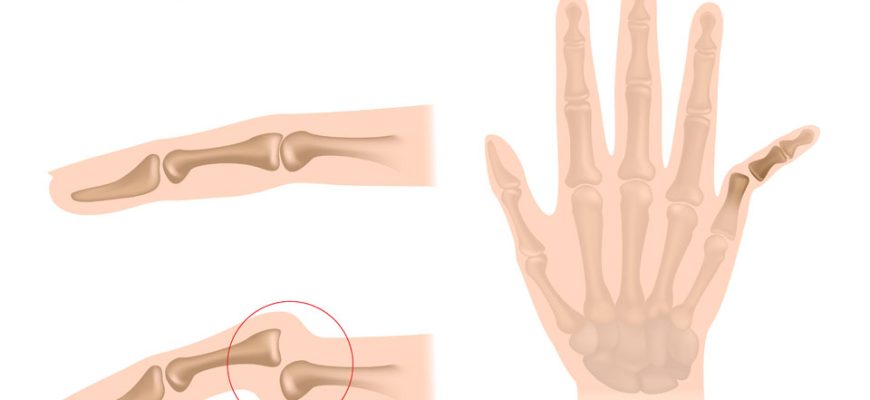
A dislocation in the wrist or fingers occurs when a strong force causes the bones in a joint to become misaligned or completely separated. The bones are forced out of their normal position, which causes significant damage to the surrounding ligaments, tendons, and sometimes nerves and blood vessels. These are serious injuries that require prompt medical attention to restore function and prevent long-term complications like stiffness, weakness, or arthritis.
Types:
Dislocations are classified by their location and severity.
Wrist Dislocations:
- Perilunate Dislocation: A severe injury where the carpal bones around the lunate (a central wrist bone) are dislocated. This is often associated with fractures.
- Lunate Dislocation: A more severe variant where the lunate itself is dislocated, usually forward into the carpal tunnel, and can compress the median nerve.
- Distal Radioulnar Joint (DRUJ) Dislocation: Dislocation of the joint between the radius and ulna bones at the wrist. Often occurs with fractures (Galeazzi injury).
Finger Dislocations (Most Common):
- PIP Joint Dislocation: The proximal interphalangeal joint (the middle knuckle) is the most commonly dislocated joint in the body. It can dislocate backward (dorsally), forward (volarly), or sideways.
- DIP Joint Dislocation: Dislocation of the distal interphalangeal joint (the joint near the fingertip) is less common.
- MCP Joint Dislocation: Dislocation of the metacarpophalangeal joint (where the finger meets the palm). Dislocation of the thumb MCP joint is a serious injury often involving a trapped tendon (Gamekeeper’s thumb).
Symptoms:
- Severe, immediate pain at the joint.
- Visible deformity (the finger or wrist may look crooked, bent, or shortened).
- Significant swelling and bruising that develops quickly.
- Inability to move the affected joint.
- Numbness or tingling (a sign of nerve impingement, especially common with severe wrist dislocations).
- The skin may appear pale or white if blood flow is compromised.
Diagnosis:
- Physical Examination: A doctor will assess the deformity, check skin color and sensation, and evaluate pulses (capillary refill) to ensure no vascular damage.
- X-rays: Essential and required. They confirm the type of dislocation and reveal any associated fractures. X-rays are taken before and after the joint is reduced (put back in place).
- CT Scan or MRI: May be used for complex wrist dislocations to get a detailed view of the damage to bones and ligaments for surgical planning.
Prevention:
- Use protective gear like gloves or wrist guards for sports (basketball, football, skiing) and high-risk activities.
- Practice proper technique in sports to avoid jamming fingers.
- Fall prevention strategies to avoid landing on an outstretched hand.
Treatment:
- Immediate (Reduction): The dislocated joint must be put back into place (closed reduction). This should be done by a medical professional with local anesthesia. Never try to pop it back in yourself, as this can trap tendons or cause further damage.
- Post-Reduction: After reduction, the joint is immobilized with a splint or buddy taping (for simple finger dislocations).
- Physical Therapy: Critical for recovery. Therapy focuses on reducing swelling, restoring range of motion, and strengthening the joint to prevent stiffness and future instability.
Types of Surgeries:
Surgery is required if the dislocation is unstable, cannot be reduced closed, or is associated with significant ligament damage or fractures.
- Open Reduction and Internal Fixation (ORIF): Used for fracture-dislocations. The surgeon makes an incision to realign the bones and uses pins, screws, or plates to hold them in place.
- Ligament Repair/Reconstruction: For dislocations with complete ligament tears (e.g., thumb UCL repair for “Gamekeeper’s thumb” or volar plate repair in fingers).
- Closed Reduction and Percutaneous Pinning (CRPP): The joint is reduced closed, and then temporary pins are inserted through the skin to hold the bones in place while ligaments heal.
Prognosis:
- With prompt and proper treatment, the prognosis is generally good.
- Stiffness is the most common complication, especially if immobilized for too long.
- Instability or Arthritis: If the injury is severe or doesn’t heal properly, the joint may remain loose or develop post-traumatic arthritis years later.
- Recovery can take several weeks to months, and full strength and motion may not completely return.
Warning Signs & When to Consult a Doctor:
You must see a doctor for any suspected dislocation.
Go to the Emergency Room or an urgent care clinic immediately if you experience:
- A visibly deformed finger or wrist after an injury.
- Severe pain and inability to move the joint.
- Numbness or tingling in the fingertip (a sign of nerve injury).
- The finger is cold, pale, or blue (a sign of vascular injury—this is a medical emergency).
- The skin is broken near the dislocated joint (an open dislocation).