Systemic Lupus Erythematosus, commonly known as lupus, is a chronic autoimmune disease in which the body’s immune system attacks its own tissues and organs. Unlike gout, which primarily affects joints, lupus can cause inflammation that damages many different body systems, including your joints, skin, kidneys, blood cells, brain, heart, and lungs.
What It Is
Lupus is characterized by a loss of self-tolerance, meaning the immune system fails to distinguish between foreign invaders (like viruses and bacteria) and the body’s own healthy tissues. This leads to widespread inflammation and tissue damage. The course of lupus is often unpredictable, with periods of illness (flares) and periods of wellness (remission).
Causes & Risk Factors
The exact cause of lupus is unknown, but it’s believed to result from a combination of genetic, hormonal, and environmental factors.
- Genetics: No single “lupus gene” exists, but certain genetic variations can increase susceptibility. Having a family member with lupus or another autoimmune disease raises your risk.
- Hormones: Lupus is more common in women (90% of cases), particularly during childbearing years, suggesting a link to estrogen.
- Environmental Triggers: These can initiate the disease or cause a flare. Common triggers include:
- Sunlight (UV light exposure)
- Infections
- Certain medications (drug-induced lupus, which is usually reversible)
- Physical or emotional stress
- Smoking
Symptoms
Lupus is called “the great imitator” because its signs and symptoms can mimic those of other ailments. They vary widely from person to person and can include:
- Fatigue: Extreme and persistent tiredness is one of the most common symptoms.
- Fever: Often a low-grade fever without a clear cause.
- Joint Pain, Stiffness, and Swelling: Affecting multiple joints, similar to arthritis.
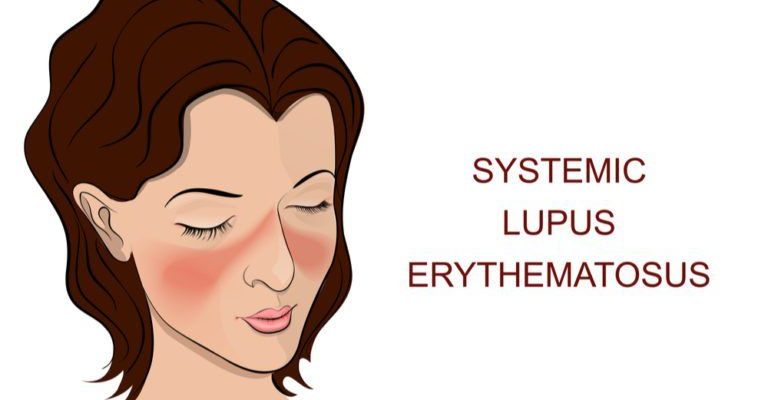
- Butterfly-shaped Rash (Malar Rash): A classic sign—a rash over the cheeks and bridge of the nose.
- Skin Lesions: Worsen with sun exposure.
- Chest Pain: Especially when taking a deep breath, from inflammation of the lung lining (pleurisy) or heart lining (pericarditis).
- Hair Loss: Patchy or general.
- Kidney Problems (Lupus Nephritis): A serious complication, often showing no early symptoms but detected via urine tests.
- Neurological Symptoms: Headaches, confusion, memory loss, and seizures.
- Raynaud’s Phenomenon: Fingers and toes turning white or blue in response to cold or stress.
Diagnosis
Diagnosing lupus can be challenging because it develops slowly and symptoms vary. There is no single diagnostic test. Doctors use a combination of:
- Medical History and Physical Exam: A detailed account of symptoms and a physical check for common signs.
- Blood Tests:
- Antinuclear Antibody (ANA) Test: A positive ANA is found in most people with lupus but can also be positive in other conditions. It is a screening test, not a confirmation.
- Other Antibody Tests: Anti-dsDNA, Anti-Smith (Anti-Sm) are more specific for lupus.
- Complement Levels: Low levels of complement proteins (C3, C4) indicate active disease.
- Urine Tests: To check for protein or blood, which can signal kidney involvement.
- Biopsy: Often of the skin or kidneys, to confirm the diagnosis and assess damage.
Treatment
There is no cure for lupus, but treatments can help control symptoms, prevent flares, and minimize organ damage. Treatment is highly individualized and may include:
- Lifestyle Modifications: Sun protection (sunscreen, protective clothing), a balanced diet, regular exercise, and stress management.
- Medications:
- NSAIDs: For pain and fever.
- Antimalarial Drugs: Hydroxychloroquine (Plaquenil) is a cornerstone treatment that helps control disease activity and prevent flares.
- Corticosteroids: (e.g., Prednisone) to quickly reduce inflammation during flares.
- Immunosuppressants: (e.g., Methotrexate, Azathioprine, Mycophenolate) for severe cases, especially with major organ involvement.
- Biologics: Belimumab (Benlysta) is a targeted therapy that specifically calms the overactive immune system in lupus.
Prevention
Since the cause is not fully understood, lupus cannot be prevented. However, once diagnosed, you can take steps to prevent flares:
- Attend all medical appointments.
- Get adequate rest.
- Wear sunscreen and sun-protective clothing daily.
- Exercise regularly.
- Don’t smoke.
- Take medications as prescribed.
Prognosis
The prognosis for lupus has improved dramatically over the past 50 years. With modern treatment, most people with lupus can lead full, active lives. However, it remains a serious disease. The prognosis depends on the severity of the disease and which organs are involved. Early diagnosis and proper treatment are crucial for improving long-term outcomes.
When to See a Doctor
You should see a doctor if you develop an unexplained rash, ongoing fever, persistent aching, or overwhelming fatigue, especially if you have more than one of these symptoms. If you have already been diagnosed with lupus, contact your doctor if you notice any new or worsening symptoms that could indicate a flare.