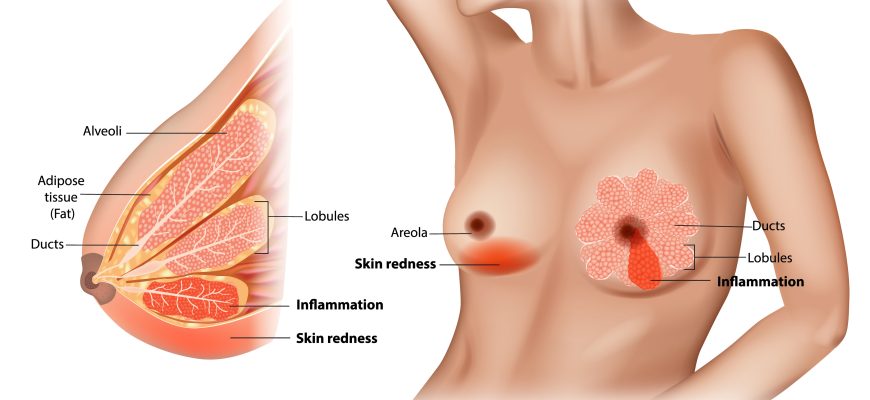
Mastitis is an inflammation of breast tissue, often caused by infection or milk stasis. It commonly affects breastfeeding women (lactational mastitis) but can also occur in non-breastfeeding individuals (non-lactational mastitis).
Causes
1. Lactational Mastitis
- Milk stasis (blocked milk duct → bacterial growth)
- Bacterial infection (Staphylococcus aureus most common)
- Poor breastfeeding techniques (incomplete emptying, cracked nipples)
2. Non-Lactational Mastitis
- Smoking-related duct damage (periductal mastitis)
- Chronic inflammation (granulomatous mastitis)
- Breast piercings/trauma
Risk Factors
✔ Breastfeeding (especially first 6 weeks)
✔ Cracked/sore nipples (bacteria entry point)
✔ Insufficient milk drainage (skipped feeds, tight bras)
✔ Weakened immunity (stress, fatigue, malnutrition)
✔ Diabetes/smoking (increases non-lactational risk)
Symptoms
- Breast pain, swelling, warmth (usually one-sided)
- Red, wedge-shaped area on the breast
- Fever & chills (if infection present)
- Flu-like fatigue & body aches
- Pus discharge (if abscess forms)
Types of Mastitis
| Type | Causes | Common in |
|---|---|---|
| Lactational | Milk stasis, bacterial infection | Breastfeeding moms |
| Periductal | Smoking, duct inflammation | Non-breastfeeding women |
| Granulomatous | Autoimmune-like reaction | Younger women (rare) |
| Infectious abscess | Untreated mastitis → pus collection | Severe cases |
Diagnosis
- Clinical exam (redness, swelling, fever)
- Ultrasound (checks for abscess)
- Milk culture (if recurrent/unresponsive to antibiotics)
- Biopsy (if granulomatous mastitis suspected)
Treatment
1. Lactational Mastitis
- Continue breastfeeding/pumping (prevents milk stasis)
- Warm compresses & massage (helps unblock ducts)
- Antibiotics (dicloxacillin, cephalexin for 10-14 days)
- Pain relief (ibuprofen, acetaminophen)
2. Non-Lactational Mastitis
- Antibiotics (if infected)
- Steroids (for granulomatous mastitis)
- Surgery (drain abscess or remove damaged ducts)
3. Abscess Treatment
- Needle aspiration or incision & drainage
- IV antibiotics if severe
Complications
- Breast abscess (pus pocket requiring drainage)
- Recurrent infections (if underlying issue persists)
- Early weaning (due to pain/discomfort)
- Sepsis (rare, if untreated)
Prevention
✔ Proper breastfeeding technique (latch, positioning)
✔ Avoid long gaps between feeds
✔ Treat cracked nipples (lanolin cream)
✔ Wear loose bras (no tight compression)
✔ Quit smoking (reduces non-lactational risk)
Prognosis
- Improves in 2-3 days with antibiotics + milk drainage
- Abscesses heal within 1-2 weeks post-drainage
- Recurrence possible if risk factors remain
When to See a Doctor?
- Fever >101°F (38.3°C)
- No improvement in 48 hours
- Pus/blood in milk
- Hard, painful lump (possible abscess)