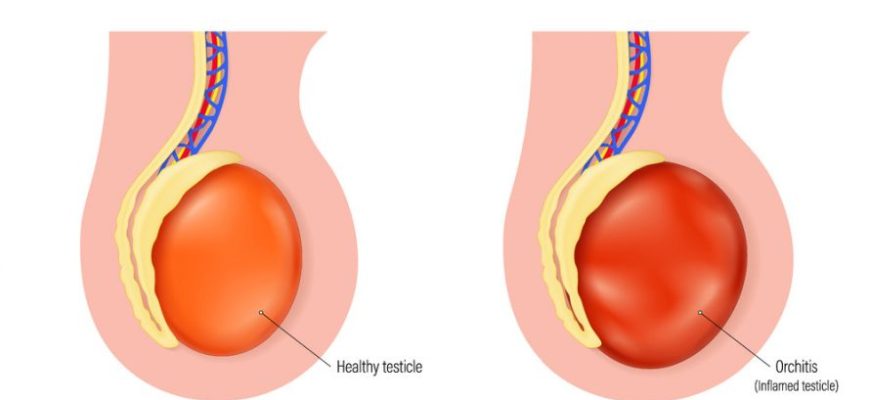
Orchitis is the inflammation of one or both testicles (testes). It can occur due to various reasons, including infections and other underlying conditions.
Etiology and Causes
- Infectious Causes:
- Viral Infections: The most common viral cause is the mumps virus, especially in males who have not been vaccinated.
- Bacterial Infections: Common bacteria include those responsible for sexually transmitted infections (STIs), such as:
- Chlamydia trachomatis
- Neisseria gonorrhoeae
- Other bacterial causes can include urinary tract infections (UTIs) or epididymitis.
- Non-Infectious Causes:
- Injury or trauma to the testicles.
- Medical procedures such as vasectomy or catheterization.
- Certain chronic diseases, like diabetes.
Risk Factors
- Unvaccinated Individuals: Lack of vaccination against diseases like mumps.
- Sexually Active Males: Especially those with multiple partners.
- Urinary Tract Infections: History of UTIs or reproductive infections.
- Age: Most prevalent in males between ages 14 and 35.
- Use of Certain Drugs: Some medications can increase the risk.
Symptoms
- Pain and swelling in one or both testicles.
- Tenderness in the affected area.
- Redness and warmth of the skin over the testicle.
- Fever and chills.
- A feeling of heaviness in the affected testicle.
- Sometimes, nausea and vomiting.
- In cases of STIs, symptoms may include discharge and painful urination.
Diagnosis
- History and Physical Examination: Assessment of symptoms, sexual history, and medical history.
- Laboratory Tests:
- Urine Analysis: To check for infection.
- Urethral Swab: To detect STIs.
- Blood Tests: To check for signs of infection and assess immune function.
- Imaging Studies:
- Ultrasound: To visualize the testicles and evaluate for swelling, abscesses, or other abnormalities.
Treatment
- Bacterial Orchitis:
- Antibiotics: Appropriate antibiotics for the specific bacteria causing the infection.
- Viral Orchitis:
- Supportive Care: Pain relief (analgesics), anti-inflammatory medications, and rest. Typically, viral orchitis is self-limiting.
- Supportive Measures:
- Ice packs to reduce swelling.
- Supportive underwear to relieve discomfort.
- Bed rest and hydration.
Prevention
- Vaccinations: Vaccination against mumps can reduce the risk of viral orchitis.
- Safe Sex Practices: Using condoms and having regular STI screenings can help reduce the risk of sexually transmitted causes.
- Hygiene: Good hygiene can help prevent urinary tract infections.
- Prompt Treatment of Infections: Address any signs of urinary or reproductive infections early.
Complications
- Abscess Formation: Pus can accumulate in the affected area.
- Testicular Atrophy: Shrinkage of the affected testicle, potentially affecting fertility.
- Infertility: Particularly associated with orchitis following mumps infection.
- Chronic Pain: Persistent discomfort in the testicular region.
- Spread of Infection: Bacteria can potentially spread to other areas, leading to more severe health issues.