What Is Retinal Detachment?
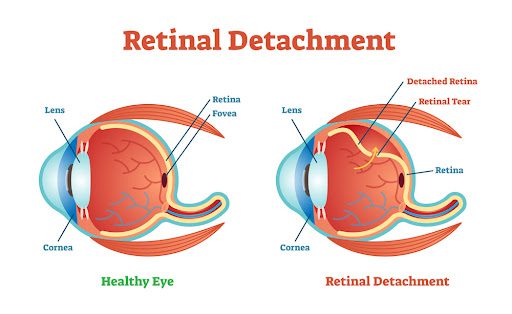
Retinal detachment occurs when the retina (the light-sensitive layer at the back of the eye) pulls away from its normal position, cutting off its blood supply. This is a medical emergency that can lead to permanent vision loss if not treated quickly.
Key Facts (National Eye Institute [NEI]):
✔ Affects 1 in 10,000 Americans yearly.
✔ Most common in adults over 50, but can happen at any age.
✔ 60% of cases are due to retinal tears (rhegmatogenous detachment).
Types of Retinal Detachment (American Academy of Ophthalmology [AAO])
- Rhegmatogenous (Most Common)
- Caused by a tear or hole in the retina, allowing fluid to seep underneath.
- Risk factors: Aging, severe nearsightedness, eye trauma, prior eye surgery.
- Tractional
- Occurs when scar tissue pulls the retina away (common in diabetic retinopathy).
- Exudative (Serous)
- Fluid builds up under the retina without a tear (due to inflammation, injury, or tumors).
Symptoms (Mayo Clinic)
Warning Signs (Seek IMMEDIATE Care If You Experience These):
✔ Sudden flashes of light (like lightning streaks, especially in peripheral vision).
✔ New floaters (black spots, cobwebs, or squiggly lines).
✔ Shadow or curtain effect over part of your vision.
✔ Blurred or distorted vision (straight lines appearing wavy).
✔ Sudden vision loss (if detachment affects the macula).
Painless condition – the absence of pain doesn’t mean it’s not serious!
Diagnosis (AAO)
- Dilated Eye Exam – Ophthalmologist checks for retinal tears/detachment.
- Optical Coherence Tomography (OCT) – Detailed imaging of retinal layers.
- Ultrasound Imaging – Used if bleeding obscures the retina.
Treatment (NEI & AAO)
Retinal Tears (Before Detachment):
- Laser (Photocoagulation) or Freezing (Cryotherapy) to seal the tear.
Detachment Repair (Surgical Options):
- Pneumatic Retinopexy – Gas bubble injected to push retina back in place.
- Scleral Buckle – A silicone band is placed around the eye to support the retina.
- Vitrectomy – Removal of vitreous gel to reattach the retina.
Recovery Time: Weeks to months, depending on severity.
Prevention (CDC & AAO)
Get regular eye exams (especially if nearsighted, diabetic, or with family history).
Protect eyes from trauma (wear safety goggles during sports/construction work).
Control diabetes & high blood pressure (to prevent tractional detachment).
Know the warning signs (flashes/floaters = emergency).
Red Flags: When to See a Doctor
GO TO THE ER OR EYE DOCTOR IMMEDIATELY IF:
- Sudden increase in floaters/flashes.
- Dark curtain blocking part of your vision.
- Blurry central vision (macula involvement).
- Recent eye trauma followed by vision changes.
Time Matters: The longer the retina stays detached, the higher the risk of permanent blindness.