Aseptic Necrosis of the Femoral Head: A Comprehensive Guide
What It Is
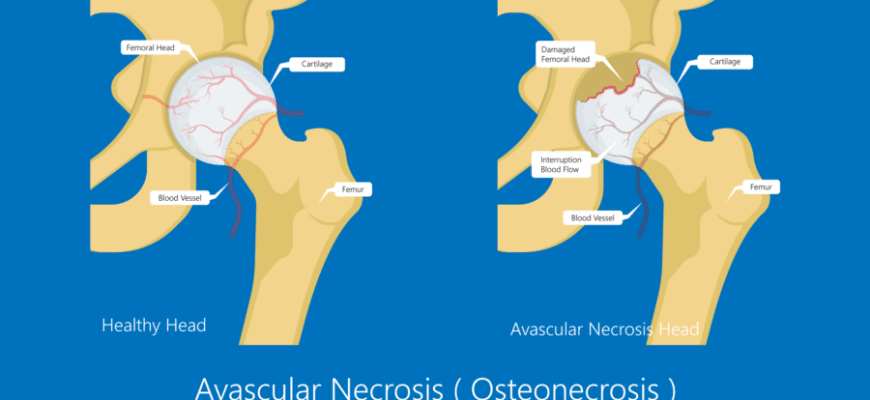
Aseptic Necrosis (AVN) of the femoral head, also known as osteonecrosis or avascular necrosis, is a disease characterized by the death of bone tissue in the ball portion (femoral head) of the hip joint. The term “aseptic” means there is no infection involved. The condition occurs when the blood supply to the femoral head is disrupted. Without adequate blood flow, the bone begins to die and can eventually collapse, leading to severe arthritis and destruction of the hip joint.
Types & Stages
AVN is not typically classified into “types” but rather into stages that describe its progression (most commonly using the Ficat and Arlet system or the Steinberg system):
- Stage 0: No symptoms, normal X-ray. Pre-clinical. May be detected incidentally by MRI.
- Stage I: Early disease. Abnormal MRI shows necrosis, but X-ray appears normal. There may be mild pain.
- Stage II: The bone begins to die, but the femoral head is still intact and round. X-rays show changes like cysts or sclerosis (hardening). Pain is more noticeable.
- Stage III: Collapse. The dead bone can no longer support the joint, and the smooth, round femoral head flattens (subchondral collapse). This is a critical turning point. X-ray clearly shows a “crescent sign.” Pain and stiffness are significant.
- Stage IV: Advanced disease. The collapsed femoral head has destroyed the articular cartilage, leading to severe osteoarthritis of the hip joint. The joint space is narrowed on X-ray.
Symptoms
Symptoms often begin gradually and worsen over time:
- Groin Pain: The most common and characteristic symptom. Pain is typically felt deep in the groin area.
- Pain Radiating to the Thigh or Buttock: Pain can travel down the front of the thigh or be felt in the buttock.
- Pain with Weight-Bearing: Pain is exacerbated by putting weight on the hip and walking.
- Limited Range of Motion: Stiffness and decreased ability to move the hip, particularly rotating it or pulling the leg inward.
- Limping (Antalgic Gait): To avoid putting pressure on the painful hip.
- Pain at Night: Pain can persist even at rest in later stages.
Diagnosis
- Medical History and Physical Exam: A doctor will assess risk factors and manipulate the hip to check for pain and limited motion.
- X-rays: Standard first imaging test. They are normal in early stages but show bone collapse, flattening, and arthritis in later stages.
- Magnetic Resonance Imaging (MRI): The gold standard for early diagnosis. An MRI can detect AVN long before it is visible on an X-ray, making it crucial for staging and planning treatment.
- Bone Scan: Less common now due to the superiority of MRI, but can sometimes be used to detect areas of abnormal bone activity.
Prevention
Prevention focuses on managing risk factors, though not all cases can be prevented:
- Limit Alcohol Consumption: Heavy drinking is a major risk factor.
- Monitor Corticosteroid Use: If you require long-term, high-dose steroid treatment for another condition, work with your doctor to use the lowest effective dose for the shortest possible time.
- Manage Underlying Conditions: Proper treatment for conditions like sickle cell disease, lupus, and hypercoagulability can reduce risk.
- Avoid Tobacco: Smoking impairs blood flow and can contribute to AVN progression.
Treatment
The goal is to preserve the natural hip joint for as long as possible and prevent collapse.
- Non-Surgical (Often used for small, pre-collapse lesions):
- Medication: NSAIDs for pain and inflammation.
- Reduced Weight-Bearing: Using crutches to take pressure off the hip. This may slow progression but is not a cure.
- Physical Therapy: To maintain range of motion and strengthen supporting muscles.
- Bisphosphonates & Statins: Some studies suggest these drugs may slow progression in early AVN, but they are not standard FDA-approved treatments.
- Electrical Stimulation: Used experimentally to try to stimulate new bone growth.
Types of Surgery
Surgery is often required, especially once collapse has begun.
- Core Decompression: The most common procedure for early-stage (pre-collapse) AVN. A surgeon drills one or more channels into the femoral head to relieve pressure, create new channels for blood vessel growth, and stimulate healing.
- Bone Grafting: Often done alongside core decompression. Bone is taken from another part of the body (autograft) or a donor (allograft) to fill the cavity and support the cartilage.
- Vascularized Fibular Graft: A more complex procedure where a segment of the fibula bone along with its blood supply is transplanted into the femoral head to provide immediate blood flow and structural support.
- Osteotomy: The bone is cut and realigned to move the damaged area of the femoral head away from the main weight-bearing zone. This is a major surgery and is less common.
- Total Hip Replacement (Arthroplasty): The definitive treatment for late-stage AVN with femoral head collapse and arthritis. The damaged ball and socket are replaced with artificial implants. This is highly successful at relieving pain and restoring function.
Prognosis
The prognosis depends heavily on the stage at diagnosis and the size of the lesion.
- Early Stage (Pre-Collapse): With interventions like core decompression, the success rate for preventing collapse and avoiding a hip replacement is good (60-80%).
- Late Stage (Post-Collapse): Once the femoral head collapses, the progression to arthritis is inevitable. The only definitive solution is a total hip replacement. THR has an excellent prognosis for pain relief and functional improvement.
- Bilateral Disease: Many patients have AVN in both hips, which complicates treatment and prognosis.
Warning Signs & When to See a Doctor
You should see an orthopedic surgeon specializing in hips if you experience:
- Persistent, deep pain in the groin area.
- Hip or groin pain that worsens with walking or standing.
- Unexplained hip pain, especially if you have any major risk factors (history of steroid use, heavy alcohol use, sickle cell disease, etc.).
- Any noticeable limp or decreased ability to move your hip.