Shoulder Fractures: A Comprehensive Guide
What it is:
A shoulder fracture is a break in any of the bones that form the shoulder girdle. This is not a single injury but a category that includes fractures of four different bones that work together to allow shoulder movement. Due to the complexity of the joint, these injuries can significantly impact arm function.
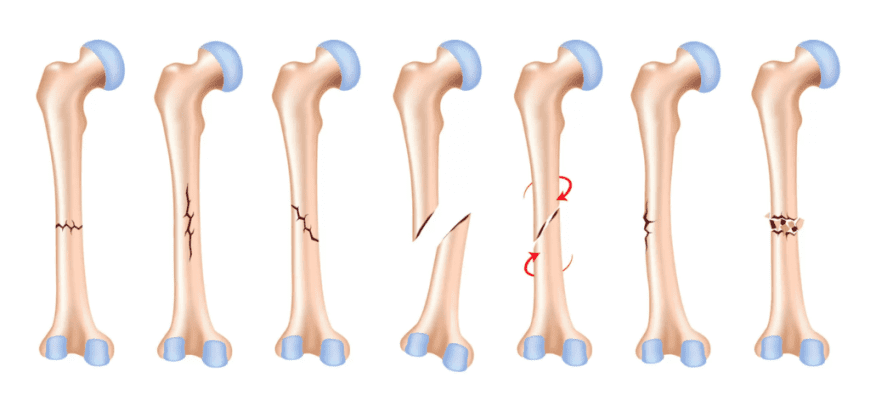
Types:
Shoulder fractures are classified by the specific bone that is broken:
- Proximal Humerus Fracture: The most common shoulder fracture. This is a break of the upper part of the arm bone (humerus), near the “ball” that fits into the shoulder socket. It is especially common in older adults with osteoporosis who fall on an outstretched hand.
- Clavicle (Collarbone) Fracture: A break in the clavicle, the long bone that connects the sternum to the shoulder. This is a very common fracture, particularly in children and young adults from falls or direct impact.
- Scapula (Shoulder Blade) Fracture: A break in the scapula, the triangular bone in the upper back. These are rare because the scapula is well-protected by muscle. When they occur, it is usually due to high-energy trauma like a car accident.
- Glenoid Fracture: The glenoid is the socket part of the shoulder joint (part of the scapula). A fracture of the socket’s rim or surface is uncommon and often associated with shoulder dislocations.
Symptoms:
- Severe, immediate pain that worsens with any arm or shoulder movement.
- Significant swelling and bruising around the shoulder, upper arm, and chest wall.
- Visible deformity (e.g., a bump or sagging of the shoulder).
- Inability to lift or move the arm without extreme pain.
- A grinding sensation (crepitus) when attempting to move.
- Tenderness to touch over the broken bone.
Diagnosis:
- Physical Examination: A doctor will assess the injury, check for deformities, and perform a critical neurovascular exam to ensure no damage to nerves or blood vessels in the arm.
- X-rays: The first and most important imaging test. They confirm the presence, location, and severity of the fracture.
- CT Scan: Often used for complex fractures, especially those involving the joint surface (like the glenoid or the head of the humerus). It provides detailed 3D images to guide treatment decisions.
- MRI: Less common for the initial diagnosis of a fracture but may be used to evaluate associated soft tissue injuries (like rotator cuff tears).
Prevention:
- Prevent Falls: Use safety gates, secure rugs, improve lighting, and hold handrails.
- Maintain Bone Health: Ensure adequate calcium and Vitamin D intake to combat osteoporosis.
- Use Protective Gear: Wear appropriate, well-fitting pads for contact sports (e.g., football, hockey).
- Wear a Seatbelt: Crucial for preventing high-energy trauma from vehicle accidents.
Treatment:
Treatment depends heavily on which bone is broken and the pattern and displacement of the fracture.
- Non-Surgical Treatment: Used for fractures that are non-displaced or minimally displaced (the bone pieces are still in good position).
- Sling or Shoulder Immobilizer: Worn for several weeks to support the arm, manage pain, and allow healing to begin.
- Medication: Pain management with NSAIDs (e.g., ibuprofen) or acetaminophen.
- Physical Therapy: Begins early with gentle motion exercises to prevent stiffness, progressively advancing to strengthening as healing allows.
- Surgical Treatment: Required for fractures that are displaced, unstable, or involve the joint surface.
- Indications: Severe displacement, open fractures (bone breaks the skin), fractures associated with nerve or vascular injury, and “fracture-dislocations.”
Types of Surgeries:
- Open Reduction and Internal Fixation (ORIF): The most common procedure. The surgeon repositions the bone fragments into their normal alignment and secures them with hardware.
- Plates and Screws: Used for fractures of the proximal humerus and clavicle.
- Intramedullary Rodding: A rod inserted down the center of the humerus for certain fractures.
- Shoulder Arthroplasty (Joint Replacement): Used for severe, comminuted (shattered) fractures of the proximal humerus, especially in older patients with osteoporosis where reconstruction is not possible. This can be a partial or total replacement.
- Hemiarthroplasty: Replacing only the “ball” part of the ball-and-socket joint.
Prognosis:
- Non-Surgical: With proper immobilization and rehabilitation, most non-displaced fractures heal well with good functional outcomes, though some stiffness is common initially.
- Surgical: The goal of surgery is to restore anatomy to allow for the best possible function. Recovery is longer and requires a dedicated course of physical therapy. Full recovery can take 4-6 months or longer.
- Potential Complications: Include stiffness (frozen shoulder), post-traumatic arthritis, malunion (healing in a bad position), nonunion (failure to heal), infection, and hardware irritation.
Warning Signs & When to See a Doctor:
Seek immediate medical attention at an urgent care clinic or emergency room for any significant shoulder injury causing severe pain, deformity, or inability to move the arm.
Go to the Emergency Room immediately if you experience:
- Numbness, tingling, or a “pins and needles” feeling in the arm or hand.
- The arm or hand feels cold or turns blue or white.
- A visible break in the skin where the bone may be protruding (open fracture).
- Shortness of breath or chest pain (can be associated with scapula fractures).
These are signs of potential nerve, vascular, or other associated injuries and require urgent evaluation.