Clavicle Dislocations: A Comprehensive Guide
What it is:
A clavicle (collarbone) dislocation is a traumatic injury where one end of the clavicle is forced out of its normal position at a joint. It’s crucial to understand that the clavicle can dislocate at two different joints, making “clavicle dislocation” an umbrella term for two distinct injuries:
- Acromioclavicular (AC) Joint Separation: This is the most common type, often called a “shoulder separation.” It occurs when the outer end of the collarbone dislocates from the acromion (a part of the shoulder blade/scapula).
- Sternoclavicular (SC) Joint Dislocation: This is a much rarer and potentially more serious injury where the inner end of the collarbone dislocates from the sternum (breastbone). Posterior (backward) dislocations are considered a medical emergency.
Types and Classification:
- AC Joint Separations are graded from I to VI based on severity (Rockwood Classification):
- Grades I & II: Mild to moderate sprains without significant dislocation. Treated non-surgically.
- Grade III: A complete dislocation where the clavicle is visibly prominent. Treatment is often non-surgical but can be controversial for athletes.
- Grades IV, V, & VI: Severe dislocations where the clavicle is severely displaced, often trapped in muscle or behind the acromion. These almost always require surgery.
- SC Joint Dislocations are classified by direction:
- Anterior: The inner end of the clavicle is pushed forward. This is the most common type.
- Posterior: The inner end of the clavicle is pushed backward toward the heart, trachea (windpipe), and major blood vessels. This is a medical emergency.
Symptoms:
- AC Joint Separation:
- Pain and swelling at the very top of the shoulder.
- A visible “bump” or deformity above the shoulder.
- Tenderness to touch over the AC joint.
- Pain with arm movement, especially crossing the body or lifting overhead.
- SC Joint Dislocation:
- Severe pain at the junction of the clavicle and sternum in the front of the chest.
- Swelling and bruising.
- Anterior: A visible bump or prominence.
- Posterior: May cause a sunken appearance; can lead to difficulty breathing, swallowing, or a feeling of choking. These symptoms require immediate emergency care.
Diagnosis:
- Physical Examination: A doctor will assess the deformity, tenderness, and range of motion.
- X-rays: The primary diagnostic tool. For AC joints, special stress views (holding a weight) may be used. For SC joints, a special serendipity view (40-degree cephalic tilt) is often required.
- CT Scan: This is the gold standard for diagnosing SC joint dislocations as it provides detailed 3D images to confirm the direction of the dislocation and assess any damage to vital structures behind the sternum.
Prevention:
Prevention focuses on reducing the risk of high-impact trauma:
- Using proper protective equipment in contact sports (e.g., shoulder pads in football, hockey).
- Practicing proper falling techniques to avoid direct impact on the shoulder.
- Maintaining strength in the shoulder and upper back muscles to provide stability.
Treatment:
- Non-Surgical Treatment: This is the standard for most AC joint injuries (Grades I-III) and many anterior SC joint dislocations.
- Sling: Immobilization for 2-4 weeks to allow ligaments to heal.
- Ice and Medication: To reduce pain and inflammation.
- Physical Therapy: Critical for restoring range of motion, strength, and function once the initial pain subsides.
- Surgical Treatment: Reserved for:
- Severe AC joint separations (Grades IV, V, VI).
- Failed non-surgical treatment for lower-grade injuries that remain painful.
- Most posterior SC joint dislocations and unstable anterior dislocations.
- The goal of surgery is to reduce the dislocation (put the bone back in place) and reconstruct the torn ligaments to stabilize the joint.
Types of Surgeries:
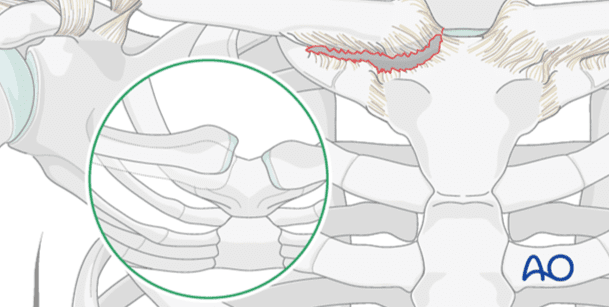
- For AC Joint Reconstruction:
- Ligament Reconstruction: Using a tendon graft (often from the patient or a donor) to recreate the coracoclavicular ligaments that stabilize the joint.
- Suture Button Technique: A minimally invasive method using strong sutures and buttons to secure the clavicle to the coracoid process (a part of the scapula).
- Hook Plate: A metal plate that screws into the clavicle and has a hook that goes under the acromion to hold the joint reduced. It is very strong but must be removed in a second surgery months later.
- For SC Joint Reconstruction:
- This is a more complex procedure due to the proximity to vital organs. It often involves a cardiothoracic or trauma surgeon.
- Techniques involve using a tendon graft to stabilize the reduced joint.
- Metal pins are avoided due to the risk of migration into the heart or major blood vessels.
Prognosis:
- AC Joint Separation: The prognosis is generally excellent. Most people with Grades I-III injuries return to full activity within 6-12 weeks with non-surgical treatment. They may have a permanent bump but often have full function. Surgical outcomes are also very good, with a high rate of return to sport, though recovery takes 4-6 months.
- SC Joint Dislocation: With proper treatment, the prognosis is good. There is a higher risk of recurrence and post-traumatic arthritis in the joint compared to AC injuries. Posterior dislocations treated promptly typically have good outcomes without long-term issues.
Warning Signs & When to See a Doctor:
You should see a doctor (an orthopedic specialist is ideal) for any significant shoulder or chest injury, especially if there is a visible deformity.
Go to the Emergency Room immediately if you experience any of the following after an injury to the base of your neck or chest:
- Difficulty breathing or shortness of breath.
- Difficulty swallowing or a feeling of choking.
- Hoarseness in your voice.
- Numbness, weakness, or swelling in your arm.
- A feeling of dizziness or lightheadedness.
These are signs of a posterior SC joint dislocation compressing vital structures and constitute a medical emergency.