1. Etiology
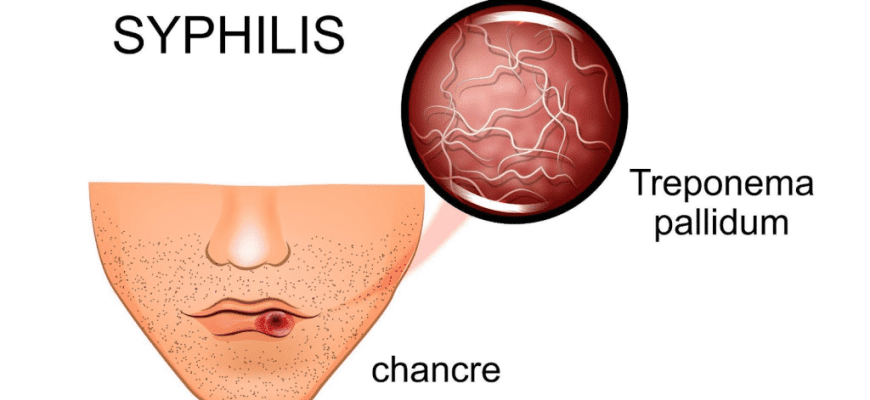
Pathogen: Treponema pallidum, a spiral-shaped bacterium from the spirochete family. Highly mobile, poorly stained by conventional methods (hence “pale” treponema). Sensitive to drying, heating, and disinfectants.
2. Transmission Routes
- Sexual (95% of cases): vaginal, anal, oral sex
- Vertical: mother to fetus (congenital syphilis)
- Blood contact: blood transfusion, shared needles
- Household (rare): through moist items (toothbrushes, tableware)
3. Symptoms by Stages
Incubation period: 3-4 weeks (range 10-90 days)
Primary syphilis (3-6 weeks):
- Chancre (painless ulcer) at infection site
- Lymph node enlargement
- Self-healing of chancre in 4-6 weeks
Secondary syphilis (6 weeks – 2 years):
- Generalized rash (roseola, papules)
- “Necklace of Venus” (neck depigmentation)
- Condylomas in anogenital area
- Fever, malaise
- Liver/kidney involvement
Tertiary syphilis (3-10 years):
- Gummas (nodules) in organs/tissues
- Neurosyphilis
- Cardiovascular complications
4. Diagnosis
- Dark-field microscopy (treponeme detection)
- Serological tests:
- Non-treponemal (RPR, VDRL) – for screening
- Treponemal (ELISA, TPHA) – confirmatory
- PCR (complex cases)
- CSF examination (for neurosyphilis)
5. Prevention
- Condom use
- Avoiding casual sex
- Prenatal screening (3 times during pregnancy)
- Preventive treatment for contacts
6. Treatment
First-line:
- Benzathine penicillin G (IM injection)
- For allergies: doxycycline, ceftriaxone
Follow-up:
- Serological tests every 3 months
- Cure confirmed by negative tests for 2 years
7. How to Recognize Syphilis?
Warning signs:
- Painless genital ulcer
- Unexplained rash on palms/soles
- Unexplained lymphadenopathy
- Patchy hair loss
8. Post-Exposure First Aid
- Clean contact area with chlorhexidine within 2 hours
- See dermatovenereologist within 48 hours
- Preventive treatment (benzathine penicillin)
- Retest after 3 weeks
9. How to Identify Syphilis in Others?
Visible signs:
- Characteristic rashes
- Multiple skin scars
- Speech/coordination problems (late stages)
- Nasal deformity (gummatous lesions)
Important: Diagnosis requires medical confirmation! Self-diagnosis is unreliable.
10. Complications
- CNS damage (general paresis)
- Aortitis, aortic aneurysm
- Gummatous organ damage
- Congenital deformities
Prognosis: Full recovery if treated early. Irreversible damage in late stages.