Heel Spurs: A Comprehensive Guide
What It Is
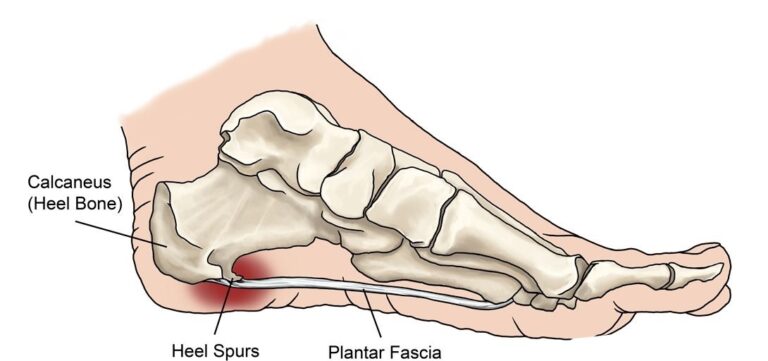
A heel spur (calcaneal spur) is a bony outgrowth that develops on the underside of the heel bone (calcaneus). It is formed by a buildup of calcium deposits over a period of many months. Contrary to popular belief, the spur itself is often not the direct cause of pain. Instead, pain is typically caused by inflammation and damage to the soft tissues near the spur, most commonly plantar fasciitis. The heel spur is a symptom of the underlying tension and inflammation, not the primary cause.
Types
Heel spurs are classified by their location on the heel bone:
- Inferior Calcaneal Spur: The most common type. It extends along the underside of the heel, where the plantar fascia ligament attaches. This is the type associated with plantar fasciitis.
- Posterior Calcaneal Spur: Located at the back of the heel, where the Achilles tendon attaches. This type is often associated with inflammation of the Achilles tendon (Achilles tendinitis).
Symptoms
Many people have heel spurs with no symptoms at all. When symptoms do occur, they are almost always due to the associated condition (like plantar fasciitis) and are indistinguishable from it:
- Sharp, stabbing pain in the bottom of the heel, especially with the first few steps in the morning or after a period of rest.
- Dull, aching pain in the heel throughout the day, often after long periods of standing or walking.
- Point tenderness when pressing on the center or front of the heel.
- Inflammation and swelling at the front of the heel.
Diagnosis
- Physical Examination: A doctor (podiatrist or orthopedist) will press on the heel to locate the tender area and rule out other causes of heel pain.
- X-ray: This is the definitive diagnostic tool. An X-ray can clearly show the bony protrusion of a heel spur. However, because many people have asymptomatic spurs, the presence of a spur on an X-ray does not automatically mean it is the source of the pain. The diagnosis is made by correlating the X-ray findings with the location of the patient’s pain.
Prevention
Prevention focuses on reducing stress and strain on the plantar fascia and heel:
- Wear Supportive Shoes: Avoid walking barefoot on hard surfaces. Choose shoes with good arch support and a cushioned heel.
- Maintain a Healthy Weight: Excess weight puts additional stress on the feet and heels.
- Stretch Regularly: Regularly stretching the calf muscles, Achilles tendon, and plantar fascia helps maintain flexibility and reduce tension.
- Replace Worn-Out Shoes: Athletic shoes lose their cushioning and support over time.
- Gradually Increase Activity: Avoid suddenly increasing the intensity or duration of your workouts.
Treatment
Treatment is almost always non-surgical and targets the inflamed tissue, not the spur itself.
- Conservative (First-Line) Treatments:
- Rest and Ice: Reducing activity and applying ice packs to the painful area.
- Stretching Exercises: Specific exercises for the plantar fascia and calf muscles.
- Orthotics/Inserts: Over-the-counter or custom shoe inserts (orthotics) can provide support and cushioning to distribute pressure evenly.
- Night Splints: Worn while sleeping to keep the plantar fascia stretched overnight.
- Physical Therapy: A therapist can teach exercises and use modalities like ultrasound.
- Medication: Over-the-counter NSAIDs (e.g., ibuprofen, naproxen) can reduce pain and inflammation.
- Advanced Non-Surgical Treatments:
- Corticosteroid Injections: A powerful anti-inflammatory injection to provide short-term relief. Repeated use can damage the plantar fascia.
- Extracorporeal Shock Wave Therapy (ESWT): Sound waves are directed at the heel to stimulate healing in the tissue.
- PRP (Platelet-Rich Plasma) Injections: Uses the patient’s own blood platelets to promote healing of the damaged tissue.
Types of Surgery
Surgery is an absolute last resort, considered only after 9-12 months of aggressive non-surgical treatment has failed.
- Plantar Fascia Release: The most common procedure. The surgeon makes a small incision and partially cuts the plantar fascia ligament to relieve tension. This can be done with a small incision (open) or with special instruments (endoscopic).
- Heel Spur Removal: This is rarely done alone. If a large spur is believed to be contributing to the problem, it may be shaved down during a plantar fascia release surgery. The primary goal is always to address the soft tissue issue.
Prognosis
The prognosis for heel pain associated with a heel spur is excellent.
- Over 90% of patients improve significantly with conservative, non-surgical treatments within several months.
- Recovery requires patience and consistency with stretching, footwear changes, and other therapies.
- Even after successful treatment, the heel spur remains on the X-ray; it is simply no longer irritating the surrounding tissue.
Warning Signs & When to See a Doctor
You should schedule an appointment with a podiatrist or orthopedic doctor if you experience:
- Heel pain that persists for more than 2-3 weeks despite home care (rest, ice, stretching).
- Severe pain and swelling in your heel.
- Pain that prevents you from walking or performing daily activities.
- Heel pain accompanied by redness, warmth, or fever (to rule out infection).
- Numbness or tingling in your heel or foot.