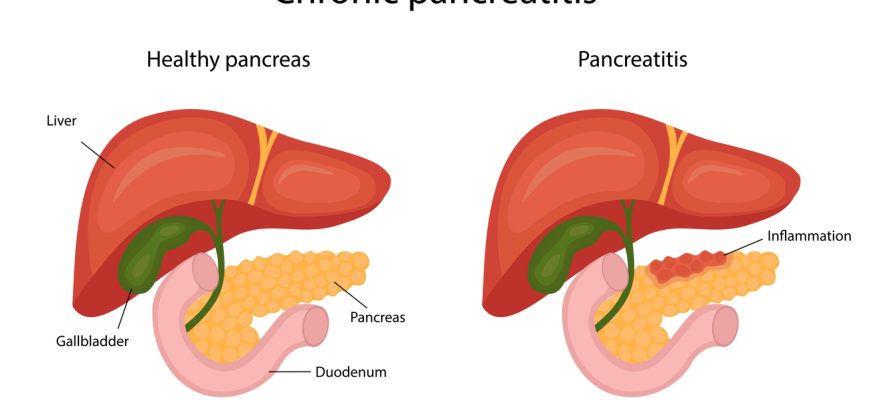
Pancreatitis is inflammation of the pancreas, an organ that produces digestive enzymes and insulin. It can be acute (sudden and short-term) or chronic (long-lasting, leading to permanent damage). Severe cases can be life-threatening.
Etiology (Causes)
1. Acute Pancreatitis
- Gallstones (most common cause, blocking the pancreatic duct)
- Heavy alcohol use (second most common cause)
- High triglycerides (especially >1,000 mg/dL)
- Certain medications (e.g., diuretics, steroids, some HIV drugs)
- Infections (mumps, hepatitis, cytomegalovirus)
- Abdominal trauma or surgery
- Autoimmune conditions
2. Chronic Pancreatitis
- Long-term alcohol abuse (70-80% of cases)
- Genetic mutations (e.g., cystic fibrosis, hereditary pancreatitis)
- Autoimmune pancreatitis
- Recurrent acute pancreatitis episodes
- Obstruction (pancreatic duct strictures, tumors)
Types
- Acute Pancreatitis
- Mild (edematous)
- Severe (necrotizing, with tissue death)
- Chronic Pancreatitis
- Calcifying (most common, with stone-like deposits)
- Obstructive (due to duct blockage)
- Autoimmune (IgG4-related disease)
Symptoms
Acute Pancreatitis
- Severe upper abdominal pain (radiating to the back)
- Nausea & vomiting
- Fever & rapid pulse
- Tenderness/swelling in abdomen
- Jaundice (if gallstones block bile duct)
Chronic Pancreatitis
- Recurrent or constant abdominal pain
- Weight loss & malnutrition (due to poor digestion)
- Oily, foul-smelling stools (steatorrhea)
- Diabetes (from damaged insulin-producing cells)
Diagnosis
- Blood tests
- Elevated amylase & lipase (3x normal = acute pancreatitis)
- Liver enzymes, triglycerides, calcium
- Imaging
- Abdominal ultrasound (checks for gallstones)
- CT scan (assesses inflammation, necrosis)
- MRI/MRCP (evaluates ducts, tumors)
- Endoscopic ultrasound (EUS) (for chronic cases)
- Stool tests (fat content in chronic cases)
Treatment
Acute Pancreatitis
- Hospitalization (IV fluids, pain control, fasting)
- ERCP (if gallstones block ducts)
- Antibiotics (if infection develops)
- Surgery (for necrotic tissue or complications)
Chronic Pancreatitis
- Pain management (NSAIDs, nerve blocks)
- Pancreatic enzyme supplements (help digestion)
- Insulin therapy (if diabetes develops)
- Surgery (drainage procedures, partial pancreas removal)
Prevention
- Limit alcohol (major preventable cause)
- Treat gallstones (if present)
- Control triglycerides (diet, medications)
- Avoid smoking (increases chronic pancreatitis risk)
- Eat a low-fat diet (reduces pancreas workload)
When to See a Doctor
- Severe, persistent abdominal pain (especially after eating/drinking)
- Jaundice (yellow skin/eyes)
- Unexplained weight loss & oily stools
- Vomiting blood or black stools
How to Avoid Pancreatitis
✔ Moderate alcohol intake (or abstain if prone to attacks)
✔ Maintain healthy weight (prevents gallstones)
✔ Treat high triglycerides early
✔ Stay hydrated (helps prevent gallstones)
✔ Avoid crash diets (sudden fat changes can trigger attacks)
Final Note:
Early treatment prevents complications like pancreatic necrosis, pseudocysts, or diabetes. If you have risk factors, regular check-ups are crucial.