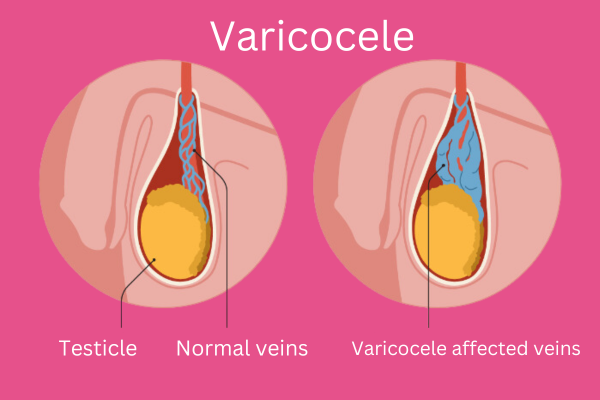
A varicocele is an abnormal enlargement of the veins within the scrotum, similar to a varicose vein that can occur in the legs. It usually affects the left side of the scrotum and is a common condition, especially among adolescent males and young adults.
Etiology
Varicoceles are primarily caused by malfunctioning valves in the veins of the spermatic cord, which is responsible for draining blood from the testicles. When these valves fail to work properly, it causes blood to pool in the veins, leading to their enlargement.
Causes and Risk Factors
- Anatomical Factors: The anatomy of the left spermatic vein, which drains into the left renal vein at a right angle, can predispose it to increased pressure and valve dysfunction.
- Age: Varicoceles often develop during puberty when increased blood flow to the testicles occurs.
- Genetics: A family history of varicoceles may increase susceptibility.
- Occupational Factors: Prolonged standing or heavy lifting may contribute to the development of varicoceles.
Symptoms
- Dull, aching pain in the scrotum that may worsen with standing or straining and improve when lying down.
- A “bag of worms” appearance due to enlarged veins in the scrotum.
- Testicular atrophy (shrinkage of the testicle).
- Decreased fertility or issues related to sperm production.
Prevention
- Maintain a healthy weight.
- Avoid prolonged standing or straining.
- Engage in regular exercise.
Diagnosis
- Physical Examination: A healthcare provider may check for a mass or abnormal veins in the scrotum, identifiable during a standing position.
- Ultrasound: A Doppler ultrasound can provide a detailed view of blood flow in the scrotal veins and confirm the diagnosis.
Treatment
- Observation: If asymptomatic or not affecting fertility, no immediate treatment may be necessary.
- Medications: Pain relievers or anti-inflammatory medications can help manage discomfort.
- Surgery: In cases of significant symptoms, infertility, or testicular atrophy, surgical intervention might be recommended:
- Varicocelectomy: Surgical removal of the affected veins.
- Embolization: A minimally invasive procedure where a catheter is used to block the abnormal vein to redirect blood flow to normal veins.
Complications
- Infertility: Varicoceles can affect sperm production and quality.
- Testicular Atrophy: Chronic blood pooling can lead to reduced testicle size.
- Recurrence: In some cases, varicoceles can recur after treatment.
Hydrocele vs Varicocele: Key Differences
1. Nature of the Condition
- Hydrocele (testicular hydrocele):
- Accumulation of serous fluid between the membranes of the testicle.
- Caused by impaired fluid production/absorption balance.
- Varicocele:
- Varicose veins of the spermatic cord (pampiniform plexus).
- Related to venous valve dysfunction causing blood stagnation.
2. Clinical Presentation
| Feature | Hydrocele | Varicocele |
|---|---|---|
| Appearance | Homogeneous scrotal swelling | “Bag of worms” (palpable dilated veins) |
| Consistency | Firm, elastic | Soft, nodular |
| Pain | Typically painless | Dull ache aggravated by exertion |
| Diurnal changes | Increases by evening | Worsens when standing |
3. Causes
- Hydrocele:
- Congenital (in children) or acquired (trauma, infections, surgery).
- Varicocele:
- Weak venous walls, hereditary factors, increased pelvic vein pressure.
4. Risks and Complications
- Hydrocele:
- Rarely causes serious issues but may lead to discomfort and scrotal deformity.
- Varicocele:
- May contribute to infertility due to testicular overheating and impaired spermatogenesis.
5. Diagnostic Methods
- Hydrocele:
- Scrotal ultrasound, transillumination.
- Varicocele:
- Doppler ultrasound (blood flow assessment), Valsalva maneuver.
6. Treatment Approaches
| Method | Hydrocele | Varicocele |
|---|---|---|
| Conservative | Observation (infants <1-2 yrs) | Scrotal support, venotonics |
| Surgical | Aspiration or Winkelmann/Lord procedure | Laparoscopic vein ligation (Marmar surgery) |
When to Seek Immediate Care?
- Hydrocele: Sudden enlargement/pain (suspected infection).
- Varicocele: Severe pain, infertility, or testicular atrophy.
Important! Both conditions require urological evaluation. Avoid folk remedies – they may worsen the problem