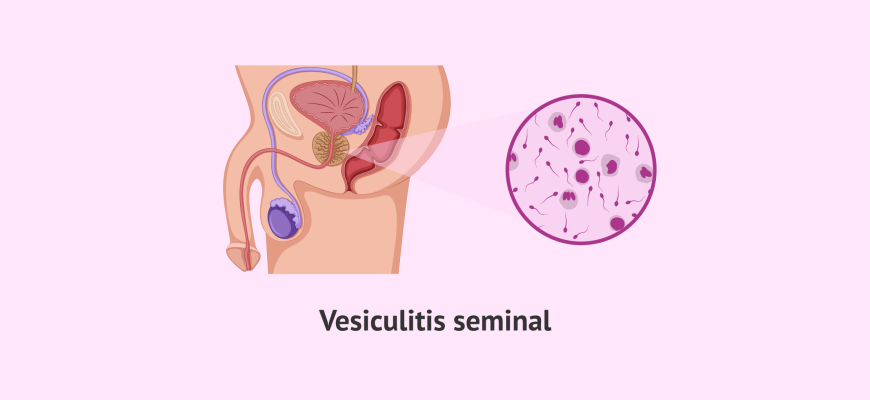
Vesiculitis, more commonly referred to as seminal vesiculitis, is an inflammation of the seminal vesicles, which are glands located behind the bladder that contribute seminal fluid to sperm during ejaculation.
Etiology and Causes
- Bacterial infections: This is the most common cause, particularly infections that ascend from the urinary tract or are related to prostatitis. Common organisms include E. coli, Enterococcus, and other uropathogens.
- Sexually transmitted infections (STIs): Pathogens such as Chlamydia trachomatis and Neisseria gonorrhoeae can lead to inflammation.
- Other infections: Viral infections, such as mumps virus, and certain tuberculosis infections can also lead to vesiculitis.
Risk Factors
- Urological conditions: Conditions such as prostatitis, urethritis, and urinary tract infections can predispose individuals to vesiculitis.
- Sexual activity: Engaging in unprotected sexual practices may increase the risk of STIs that could lead to vesiculitis.
- Age: Vesiculitis is more commonly seen in sexually active males primarily between the ages of 20 and 40.
- History of infections: A history of urinary tract or prostate infections may increase susceptibility.
Symptoms
- Pain in the lower abdomen or pelvic region
- Painful ejaculation
- Dyspareunia (painful intercourse)
- Fever and chills (in cases of acute infection)
- Pain during urination (dysuria)
- Persistent pelvic pain
- Abnormal semen (such as blood in the semen, known as hematospermia)
Diagnosis
- Clinical evaluation: Review of symptoms and medical history.
- Physical examination: A digital rectal exam may reveal tenderness in the prostate or seminal vesicles.
- Urinalysis and urine culture: This helps identify bacterial infection.
- Seminal fluid analysis: Evaluation of semen for signs of inflammation or infection.
- Imaging studies: Ultrasound or MRI may be used to visualize the seminal vesicles and rule out other conditions.
Treatment
- Antibiotics: If the cause is bacterial, appropriate antibiotics are prescribed based on culture sensitivity.
- Pain management: Nonsteroidal anti-inflammatory drugs (NSAIDs) may be used to alleviate pain.
- Sitz baths: Warm sitz baths can help relieve discomfort.
- Hydration: Increasing fluid intake can help flush out the urinary tract.
Prevention
- Safe sex practices: Using condoms to reduce the risk of STIs.
- Good hygiene: Maintaining proper genital hygiene and urinating after sexual intercourse can help reduce the risk of infections.
- Regular medical check-ups: Regular doctor visits for prostate health can help catch and manage potential infections early.
Complications
- Abscess formation: Abscesses in the seminal vesicles may develop, requiring surgical intervention.
- Chronic pelvic pain: Persistent pain may develop, affecting quality of life.
- Infertility: In severe cases, inflammation can affect seminal fluid quality and lead to fertility issues.
- Spread of infection: Infections could spread to surrounding organs, such as the prostate or bladder.